
MORE THAN FOUR MILLION Americans will undergo cataract surgery to restore vision clarity this year.1 Added clear lens replacement surgeries (refractive lens exchanges) will be performed in patients with a clear but dysfunctional, partially accommodating lens who desire surgical correction. With the high safety standards and elegance of modern-day cataract surgery, one of the biggest decisions for patients is how they want to use their eyes after surgery with respect to glasses and contact lenses. Cataract surgery for many patients is an opportunity to correct distance or distance/near vision allowing levels of independence from glasses. As clinicians we need to be armed to confidently answer the question, “What IOL do you recommend?” Two cases will be reviewed to lay out a methodical plan to answer the aforementioned question.
CASE 1
Kenneth is a 76-year-old Caucasian male who presented for a cataract evaluation. Ken’s chief concern is “blurred vision” for over 1 year with additional concerns of glare and halos during night driving. Ken has no major systemic conditions or systemic medications that should affect his surgical outcome. He uses artificial tears on an “as needed” basis.
Entering manifest refraction (MRx) is OD: +0.50-0.75x100 & OS: +0.75-1.25x068
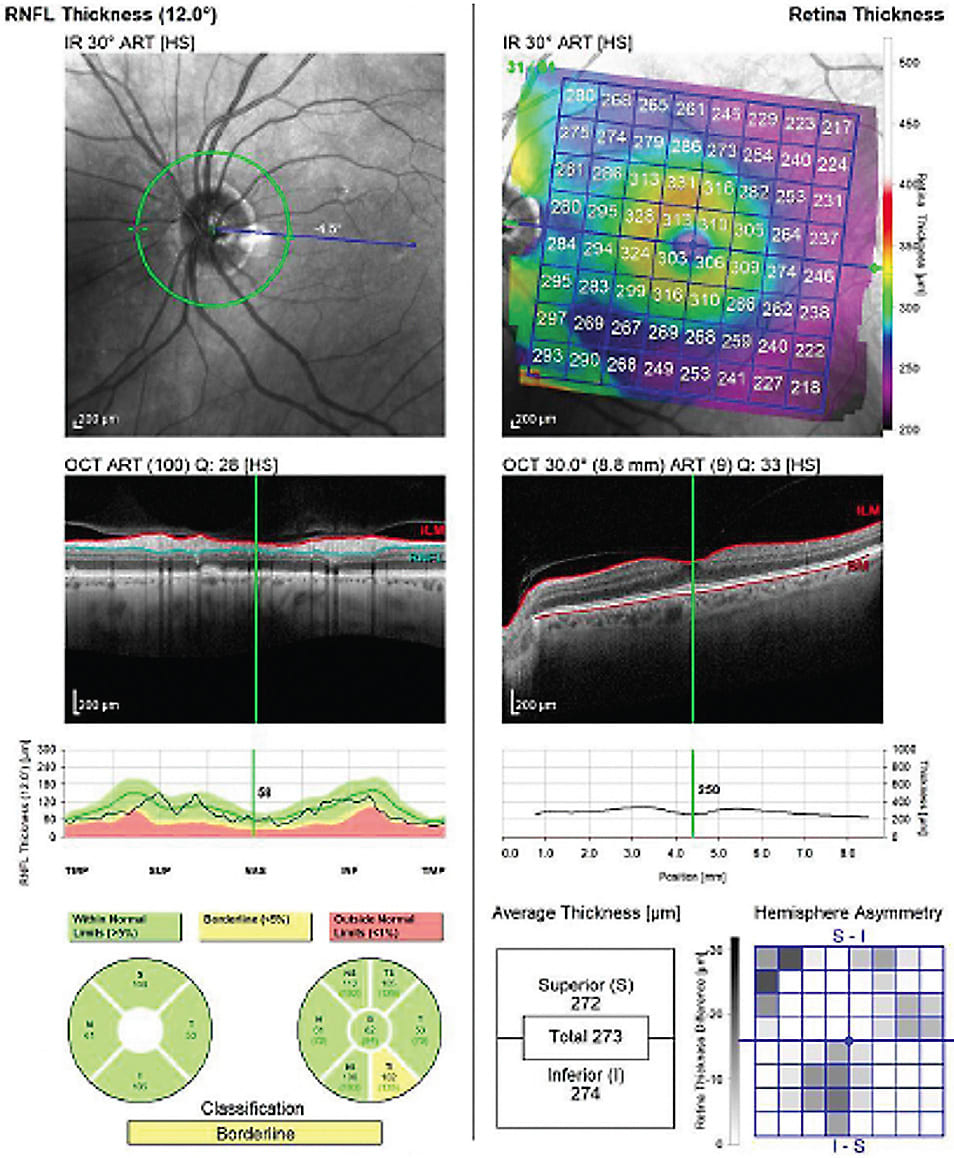
Slit lamp exam: Anterior segment was remarkable for Demodex blepharitis and meibomian gland dysfunction (MGD) in both eyes with mild-moderate nuclear sclerotic cataracts. The posterior segment was unremarkable with a vertical cup/disc ratio of 0.3v OU and a flat and clear macula OU (see Figure 1 - ONH/Mac OCT).
Step 1: Understand the demographics, habitual refraction, ocular health and biometry.
It is unfair to recommend against, or rather leave out, premium IOLs based on age, but age is important to consider. This especially is the case in younger patients (<60) having cataract surgery. This patient demographic has not experienced total presbyopia with minimal functional accommodation, and carefully educating on this point will lead to happier patients.
Second, a patient’s habitual refraction should be considered when making IOL recommendations. A near emmetropic patient commonly will have much different refractive goals than a mixed hyperopic astigmat who has worn glasses most of their life. Another habitual refraction to pay close attention to is the low myope who chooses to counteract their presbyopia by removing their glasses to read or apply make-up. This can be a terribly disappointed patient if a monofocal IOL is recommended, chosen and targeted for plano. In a study on satisfaction after multi-focal IOLs, hyperopic patients had a higher satisfaction than myopes, with the lowest satisfaction level being in patients with habitual low myopia.2
Examining ocular health with a concentration on pathology that may limit best corrected visual quantity and quality is a must before making any IOL recommendation. In many cases, treating corneal comorbidities like ocular surface disease (OSD), epithelial basement membrane dystrophy (EBMD), or mild irregular astigmatism (IA) before surgery, then reassessing biometry, will lead to improved outcomes. Finally, zeroing in on biometry can help lead physicians in the IOL discussion. Patients with greater than 0.7D of corneal astigmatism will likely benefit from astigmatism correction whether delivered with optical correction or in their IOL. Consistent biometry measurements across multiple devices also leads to confidence and better refractive outcomes.
Step 2: Listen before you recommend.
In our practice, during the counseling process before cataract surgery, all patients in some variety will be asked, “Do you prefer to wear glasses for most activities after cataract surgery, or do you prefer to gain independence from glasses?” There are many ways to ask this question, but a patient’s reply will provide a guide for our IOL recommendation.
Next, we move into daily visual tasks and goals including their occupation and hobbies. Regardless of age, our world has gone small-screen with digital devices and reading tasks, and scrutinizing near vision is important.
In Ken’s case, he’s retired and cherishes his snow-bird lifestyle in his RV. He spends his winter months fishing and golfing in Florida before driving cross-country to be grandpa the book-reader and backyard T-ball coach.
Step 3: Match the technology to the patient.
In 2021, we are spoiled with multiple IOL options that are enticing for a patient. As physicians, our job is to recommend an IOL that can meet and exceed our patient’s visual goals. There is no IOL that checks every box that our natural accommodating clear crystalline lens once did; so leveraging each IOL’s positive characteristics is key.
Ken desired as much independence from glasses at distance and near that current technologies could provide. With this in mind, our recommendation was PanOptix (Alcon) (Figure 4), a trifocal presbyopia-correcting IOL (PC-IOL).
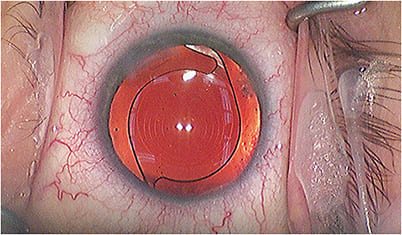
The goal for trifocality is a more continuous range of vision from distance to intermediate to near. A 2021 study published in Ophthalmology concluded that over 80% of patients with PanOptix responded “never” to requiring glasses correction, for all activities.3 Another strong option considered for this patient was Synergy (Johnson & Johnson), a diffractive IOL with a design focused on a “continuous range of vision,” according to the company.
With any lens recommendation, but heightened in the premium IOL space, setting pre-operative realistic expectations is paramount. These IOL technologies are powerful, but a pearl to keep in mind is to under-promise pre-operatively, and let the surgical outcome over-produce. With diffractive PC-IOLs, discussing post-operative glare and halos is recommended. Over time, in our experience, almost all patients will undergo neuro-adaptation, which lessens the awareness of positive dysphotopsias.
CASE 2
Heidi is a 49-year-old Caucasian female who traveled eight hours to see us for a cataract evaluation. Heidi had 8 cut radial keratotomy (RK) OD and 16 cut RK OS about 30 years ago. She later had a LASIK enhancement over her RK OD. Importantly she reports she had “very good” vision after the LASIK enhancement, and her refraction has stayed mostly stable over time.
Heidi previously showed her desire to lessen optical correction with RK, and she confirms this preference, if possible, with cataract surgery. Presently, she utilizes soft contact lenses with a monovision set-up OS for near.
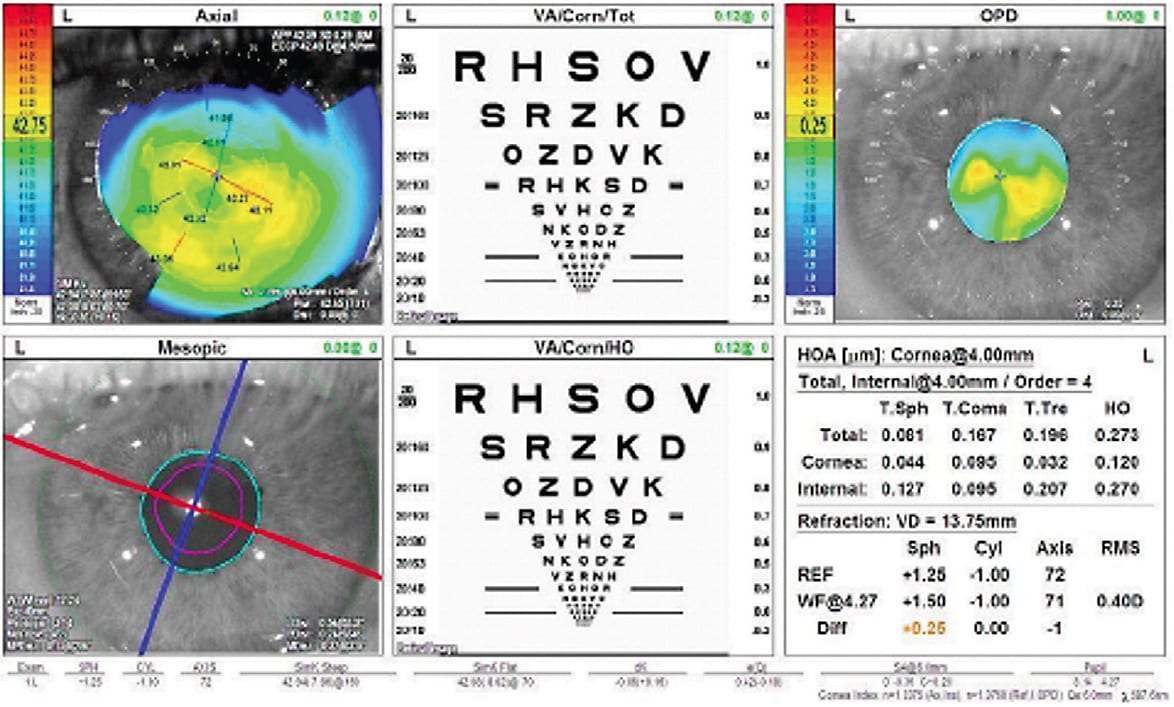
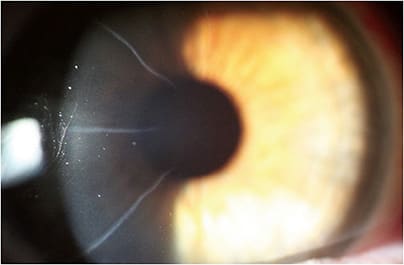
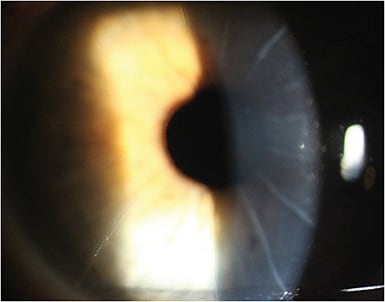
Entering MRx in both eyes is a low level of hyperopia with astigmatism in both eyes. Anterior segment exam is remarkable for 8 cut RK OD and 16 cut RK OS (Figures 5 and 6). Heidi has visually significant anterior cortical cataracts in both eyes. Posterior segment exam is unremarkable in both eyes.
Step 1: Understand the demographics, habitual refraction, ocular health and biometry.
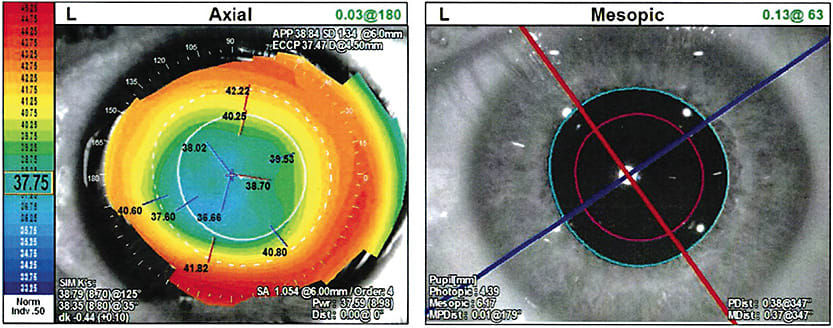
Heidi is a very active, young patient, who needs to undergo cataract surgery for her best vision. Heidi hasn’t aged into complete presbyopia yet, and for patients similar in age to Heidi, this is an important education point. Her previous RK and the amount of irregular astigmatism on the cornea/topography will help to drive the implant conversation.
Step 2: Listen before you recommend.
Heidi’s preference was to pursue premium implant options with a focus on predictability. Before her cataracts worsened, she was mostly happy with a monovision set-up in contact lenses.
Step 3: Match the technology to the patient.
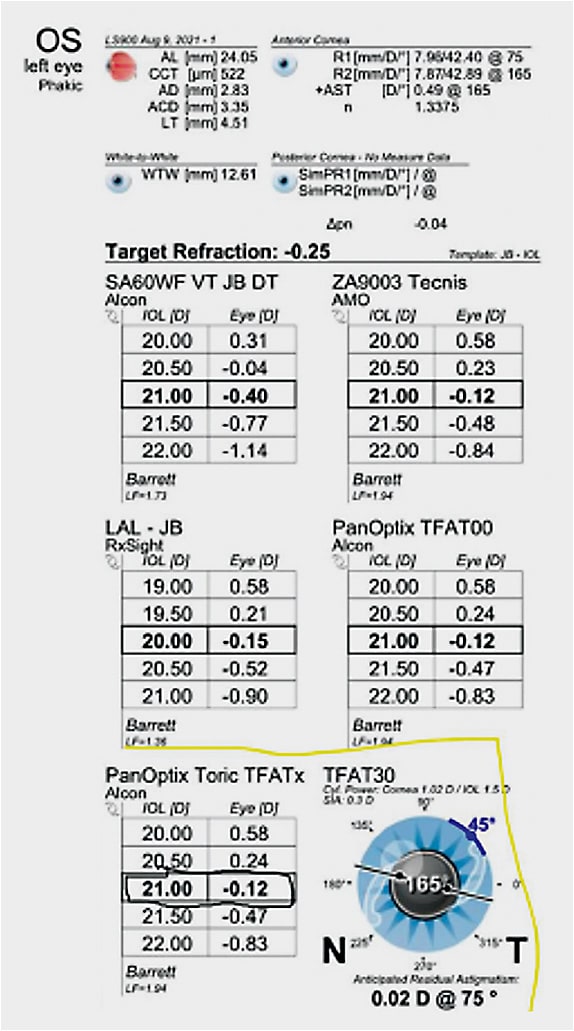
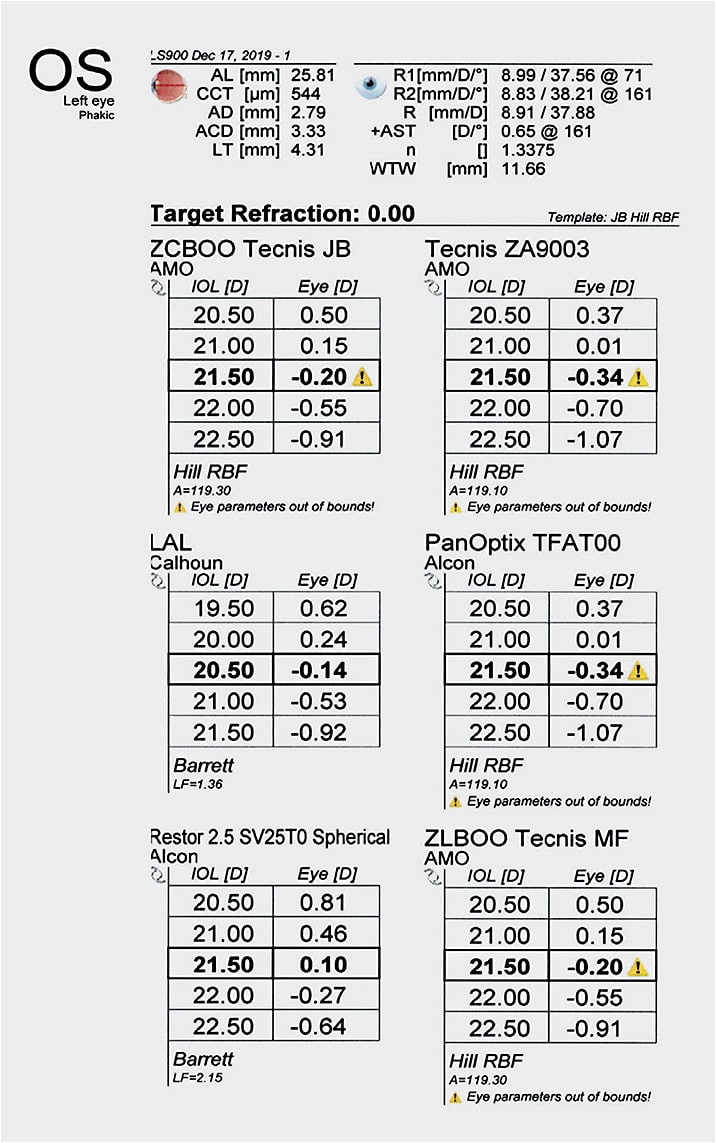
The variability in corneal curvature measurements coupled with an unstable cornea post-RK makes this recommendation a more challenging one. Thankfully, her topographic shape demonstrates a centered flattening after corneal refractive surgery with repeatable keratometry values on multiple biometry devices. Despite good quality measurements, hitting the refractive target is more challenging in patients with previous corneal surgery, and this challenge is multiplied with previous RK. Our recommendation for Heidi was to focus on good quality distance vision, have adequate intermediate vision (dashboard, computer), and use near optical correction as needed. Prioritizing predictability, we chose to do an optic adjustable IOL with the light adjustable lens (LAL, RxSight). We planned for a monovision initial target of plano OD and -1.00 residual myopia OS. With three adjustments available, these “test drives” allow Heidi to have a real-life trial of the visual set-up and we can adjust as needed.
Summary
As physicians, our patients rely on us in their moment of vulnerability before surgery to make a strong recommendation and execute the plan. With a surfeit of robust IOL technologies, the IOL recommendation serves as a precursor to our patients’ lifelong vision decision.
Over 70% of U.S. surgeons offer PC-IOLs in their practice, but patient adoption has a recent slight decrease to under 7%, according to Market Scope data.4 Despite this statistic, the appetite for near vision is unchallenged. A recent Asurion survey found Americans check their cellphone nearly 100 times per day, about once every ten minutes.5
As MDs and ODs, to achieve happy patients, the first step is understanding the PC-IOL technologies, the second step is gaining experience with PC-IOLs and the final step is confidently recommending the PC-IOL when appropriate. Whether the practice utilizes corneal enhancements (laser vision correction), optic adjustable IOLs (LAL) or a combination of both, this is essential in refractive precision and patient satisfaction. All patients after cataract surgery will demand some sort of near-vision correction, and when steps 1, 2 and 3 all match, physicians should confidently make an IOL recommendation. ■
References
- Lindstrom, R. February 10, 2021. Future of cataract surgery seems promising. Ocular Surgery News. https://www.healio.com/news/ophthalmology/20210126/future-of-cataract-surgery-seems-promising .
- Dekaris I, Gabric N, Barisic A, et al. Presbyopia Correction During Cataract Surgery with Multifocal Intraocular Lenses. In: Zilfyan A (Ed.) Difficulties in Cataract Surgery. December 2017. https://www.intechopen.com/chapters/58058 .
- Modi S, Lehmann R, Maxwell A, et al. Visual and Patient-Reported Outcomes of a Diffractive Trifocal Intraocular Lens Compared with Those of a Monofocal Intraocular Lens. Ophthalmology. 2021;128(2):197-207. doi:10.1016/j.ophtha.2020.07.015.
- U.S. Refractive Quarterly Update. Market Scope, Q3(2019), 1. https://www.market-scope.com/pages/reports/139/us-refractive-quarterly-update-q3-2019
- Asurion Press Release. Americans Check Their Phones 96 Times a Day. (2019, November 21). https://www.asurion.com/about/press-releases/americans-check-their-phones-96-times-a-day/ .










