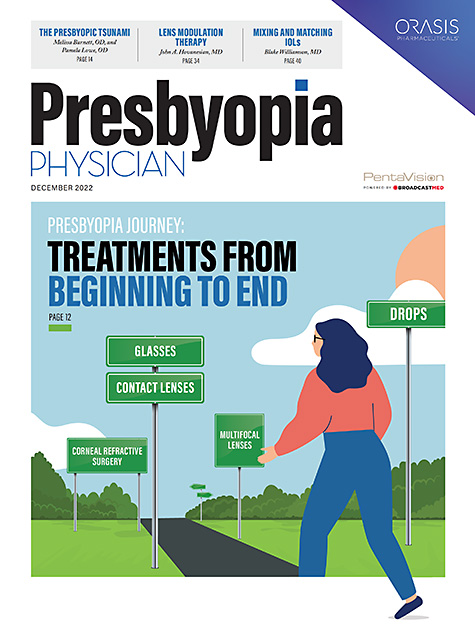
THERE IS A TANGIBLE AND URGENT NEED TO UNDERSTAND the pathogenesis of presbyopia and develop innovative technologies to improve its impact on the individual and the world economy. Contact lenses, glasses, refractive surgery, and intraocular lens surgery are the main modalities in presbyopia treatment, although they all have some disadvantages. Thus, there is an increasing need for effective, easy-to-use, and noninvasive methods to treat presbyopia while not limiting patients’ daily activities.
Of particular interest to the manifest presbyope is the advent of new devices and techniques that aim to restore the ocular accommodation of the aging eye.1 Although the most conventional treatments with eyeglasses and contact lenses for the correction of presbyopia remain dominant, in recent decades numerous surgical treatments have become available with the aim of restoring vision with good quality in a range of distances for presbyopes who have lost the capacity of accommodation.1,2
The apparent seduction of surgical methods is that the successful patient need not bother with external corrective devices, such as glasses, and can present a youthful image to the world. Unlike contact lenses, which, with translational movement and lens rotation can cause fluctuations in vision quality, there should be few problems with centering and stability after a surgical correction.1 Several technologies are being explored to achieve surgical correction of presbyopia.3-5 For example, PresbyLASIK uses the principle of laser in situ keratomileusis (LASIK) to create a multifocal corneal surface, and different approaches are available. However, with this approach, near vision is good, but far vision will be compromised.6,7
Intracorneal inlays have also been explored for the correction of presbyopia, with the advantages that no corneal tissue is removed, that it is minimally invasive, and that it can be removed; therefore, the effects are reversible.6 Nonetheless, problems with poor centration, stromal opacity, and inadequate optical performance have been reported.6
And of course the use of pharmacologic treatment for presbyopia correction is being developed as well.
True Vision Treatment
Despite all the new advances in technology, the correction of presbyopia and the restoration of accommodation remain challenges. True Vision Treatment (TVT) is a new, noninvasive technique that will change all of the expectations of presbyopic patients, who can enjoy excellent and stable near vision without the need for surgery or the daily use of pharmacologic treatments.8 The TVT technology was developed by the Yolia Health Company, based in San Diego, in collaboration with U.S. and Mexican researchers, including Dr. Alberto Osio Sancho, Dr. Charles May, Dr. Stuart Grant, Dr. John Rinehart, Dr. David Castillejos, and Dr. Raul Suarez, among others.
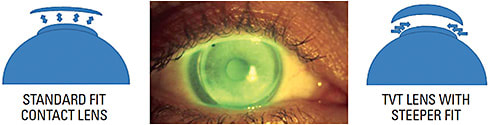
The technique is based on the principles of orthokeratology using rigid contact lenses with high oxygen permeability (rigid gas permeable; RGP), customized specifically for each patient, in combination with some ophthalmic drops, (ophthalmic solution with a base of hyaluronidase and collagenase), which function as a coadjuvant (promoting agent), for a reshaping effect of the contact lens on the cornea (Figure 1).

The solution works to maintain these changes over the longer term, even after contact lens wear has been discontinued. The RGP lens with a special design to achieve necessary molding of the cornea changes the aspheric corneal surface to a multifocal cornea. The microchanges that occur in the cornea due to the TVT lens/ophthalmic eye drop combination are the presumed mechanism of action of the TVT treatment (Figure 2).
Prospective Study
A prospective, single-site, interventional, participant-masked, 6-month study was conducted by YoliaHEALTH to evaluate the changes in uncorrected near vision before and after fitting TVT customized contact lenses in a group of 50 presbyopic patients. The RGP contact lenses were custom designed on an individual basis using corneal topography data and eccentricity values. This information was used to select the initial diagnostic lens with a specific curvature and diameter to create a unique multifocal design. Participants were evaluated before lens fitting (pre-treatment) and underwent post-treatment evaluations at 8, 15, 30, 60, 90 and 180 days.
Uncorrected high contrast logMAR near visual acuity showed a significant improvement from baseline after participants wore the customized TVT contact lenses along with using the ophthalmic solution for 7 continuous days. On average, patients had greater than 2-line improvement in uncorrected binocular near visual acuity from day 8 to day 180 (6 months) post-treatment. The results also showed that almost 70% of participants had a 2-line improvement across all visits, while 50% showed a 3-line improvement.
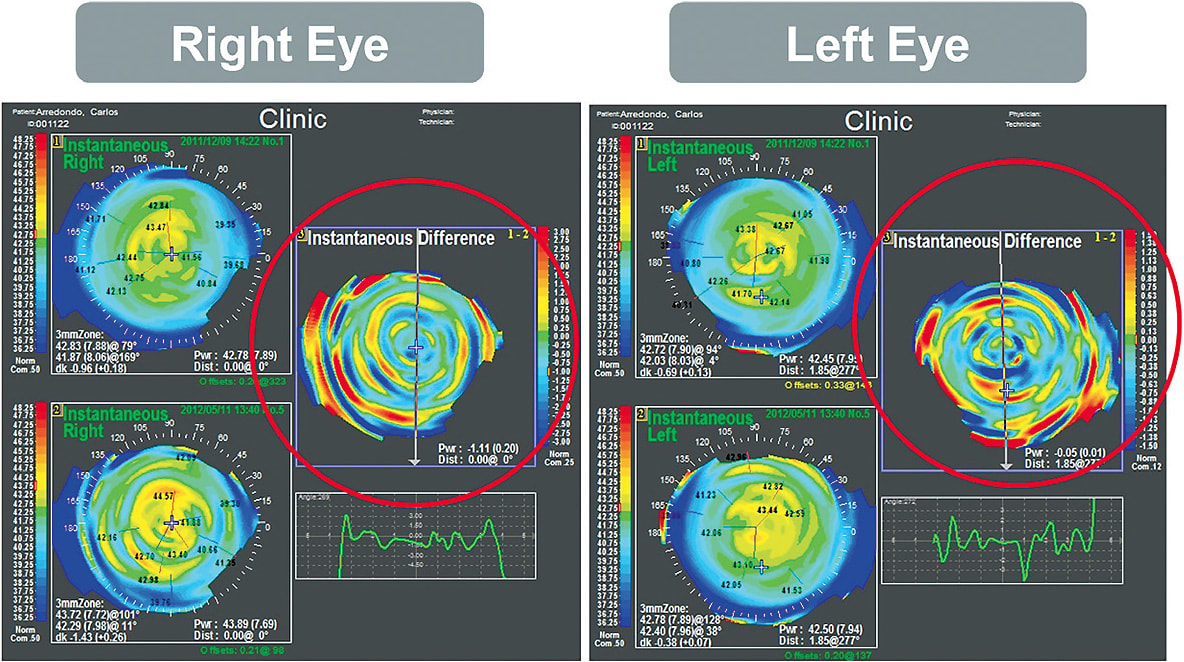
Of additional clinical relevance is that the improvement in uncorrected near visual acuity was achieved with no apparent loss of distance vision. In fact, uncorrected distance visual acuity showed an improvement of about 1 line post-TVT treatment. Therefore, it can be affirmed that the improvement in near visual acuity was obtained without any apparent compromise of overall visual function. It is important to note that the qualitative results (e.g., Pentacam difference maps) suggest that microchanges in the cornea from the lens-drop combination induce a change in the total corneal power in some regions, which may be the reason for the improved near visual acuity (Figure 3).
CONCLUSION
The normal loss of the eye’s ability to accommodate, which occurs as we age, means that people start having problems with near vision after the age of 40 and have minimum active accommodation after the age of 55. Presbyopic treatment options with spectacles and contact lenses have been available for many years and efforts continue to expand these. Improvements in technology have advanced the surgical options offering presbyopic patients a variety of approaches for the correction of their near vision.
However, although there are many choices for presbyopia management, patients eager to give up glasses might not be willing to jump into surgical correction. Currently, work is being done to fill that void with many possible noninvasive solutions. There is an increasing body of research on new approaches to help the crystalline lens accommodate, from eye drops and electrostimulation to the use of single-vision lenses of continuously variable power (liquid-filled, liquid-crystal lenses).
The encouraging results obtained in this clinical study are sufficient to demonstrate that TVT is noninvasive and can provide a significant, measurable, and sustained improvement in uncorrected near vision in presbyopic patients with no impact on distance vision or side effects. The effects of TVT treatment and the ophthalmic solution in improving near vision last for several months, which can be a great advantage compared to other treatments with shorter durations and more frequent use of pharmacologic eye drops. In addition, TVT treatment is currently being considered as a viable option for other refractive error conditions, such as myopia control and post-LASIK treatment. ■
REFERENCES
- Charman WN. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic Physiol Opt. 2014;34(4):397-426.
- Charman WN. Developments in the correction of presbyopia I. spectacle and contact lenses. Ophthalmic Physiol Opt. 2014;34(1):8-29.
- Glasser A. Restoration of accommodation: surgical options for correction of presbyopia. Clin Exp Optom. 2008;91(3):279-295.
- Dai GM. Optical surface optimization for the correction of presbyopia. Appl Opt. 2006;45(17):4184-4195.
- Ferraz CA, Allemann N, Chamon W. Phakic intraocular lens for presbyopia correction. Arq Bras Oftalmol. 2007;70(4):603-608. Portuguese.
- Vargas-Fragoso V, Alió JL. Corneal compensation of presbyopia: PresbyLASIK: an updated review. Eye Vis (Lond). 2017;4:11.
- Ong HS, Chan AS, Yau CW, Mehta JS. Corneal inlays for presbyopia explanted due to corneal haze. J Refract Surg 2018;34(5):357-360.
- True Vision Treatment. Yolia Health website. Accessed November 9, 2022. http://www.yolia.com/true-vision-treatment/
ACKNOWLEDGMENTS
We thank the clinical investigators Professor Luis Fernando Barba and Professor Ricardo Mosqueda and the administrative staff of the Optometry School at the Autonomous University of Aguascalientes in Mexico for conducting the study. We also thank Dr. Rick Potvin for the data analysis.
DECLARATIONS OF INTEREST
Alberto Osio is the founder of YoliaHEALTH. Jose Luis Monroy is an employee of YoliaHEALTH, John M. Rinehart, and Kenneth R. Kenyon are paid consultants of YoliaHEALTH.
FUNDING
This work was funded by YoliaHEALTH. Alberto Osio worked with the other authors to design the clinical study and reviewed the manuscript prior to submission.