IT WAS ESTIMATED IN 2015 that 1.8 billion people (25%) worldwide had presbyopia, a condition expected to peak by 2030.1 The population of Americans 65 and older with presbyopia is projected to roughly double between 2010 and 2050.2 Myopia is predicted to affect 49.8% of the population in 2050, posing economic burdens to society.2-6
Treatments Have Evolved
Treatment alternatives for both presbyopia and myopia have paralleled the changing epidemiological landscape. Both surgical and non-surgical treatments have progressed, but at differing speeds. Myopia was the first condition for which LASIK refractive surgery was created. Some practitioners are now successfully employing it to create monovision. The expanded indications for LASIK now include presbyopia, leading to terms like presby-LASIK.7-11
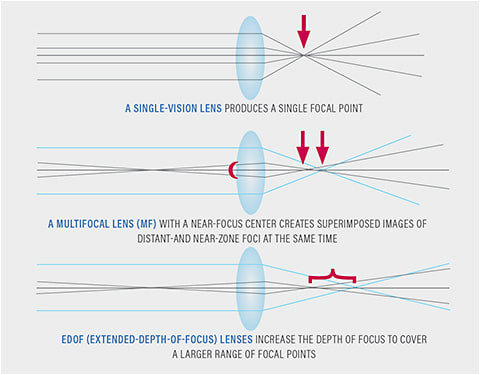
In the past, intraocular lenses (IOLs) were used only to treat spherical refractive errors. Multifocal (bifocal, trifocal, and aspheric) IOLs, as well as toric-multifocal and accommodating alternatives, are now available.12-18 Options for diffractive lenses are constantly evolving. The development of extended-depth-of-focus (EDOF) designs will be the next step, along with other alternatives such as corneal inlays. The KAMRA inlay (CorneaGen) and the Flexivue Microlens (PresbiBio) are two currently available inlays.19-21 The FDA has recalled the Raindrop Near Vision Inlay (ReVision Optics), owing to the company’s closure.
A variety of contact lens designs are available as noninvasive treatments. Multifocal designs are now available in rigid, soft, and hybrid lenses. Simultaneous and alternating designs are available for rigid lenses, whereas simultaneous designs are available for soft and hybrid lenses. Although they were effective treatments in the past, the Triton lens (Gelflex) and the first diffractive bifocal lens, Echelon (Hydron), are no longer available.23 Today, soft simultaneous vision contact lenses are available in aspheric, zonular, and EDOF designs.
Various topical pharmaceutical agents with diverse mechanisms of action have recently been released or are in development; these expand the use of depth-of-focus lenses by causing a pinhole effect or restoring some degree of flexibility to the aged crystalline lens.24
In the remainder of this article, I will provide an update on EDOF by comparing treatment options.
Optical Basics
When light from an object passes through corrective lenses and the eye’s optics, a single-point focus can be difficult to achieve. Three things can happen to a wavefront of light when it meets an optical surface: reflection, absorption, or transmittance. Individual wavelets combine to form a wavefront that is diffracted when it comes in contact with an aperture’s edge, such as the iris plane, resulting in interference. A point object’s transmitted wavefront should ideally be conjugated with a point image. With both paraxial and off-axis objects, we live in a world of polychromatic light. The wavefronts formed collide both with regular and uneven optical surfaces, resulting in aberrations: differences between the ideal and actual wavefronts. These refracting surface aberrations smear the focus light.
Lower- and higher-order aberrations can be distinguished. Lower-order aberrations make up around 90% of all aberrations in the eye and include defocus defects (myopia, hyperopia, regular astigmatism, and prism) that we correct every day with refraction.25 Higher-order aberrations account for the remaining 10% of the eye’s defects; they frequently affect the quality of vision following an optical or surgical procedure.26 Spherical aberration, coma, and trefoil are the most clinically important.27
The aberration will increase 16 times faster than the change in diameter, because spherical aberration increases as the fourth power of the pupil diameter.25 It is one of the reasons why patients with large pupils who have LASIK may have halos and can also cause night myopia in healthy eyes.26 In relation to the pupillary aperture, spherical aberration is also affected by accommodation and IOL axial location.25 Coma increases when a corneal graft, crystalline or intraocular lens, inlay, or ablation zone is decentered. Trefoil plays a modest role in image aberration.28
Reducing the smear of a point focus begins with correcting refractive defocus. Higher aberrations and visual quality are substantially influenced by the geometries of refracting surfaces, aperture size, and position of elements in an optical system, both axially and longitudinally.
Contact Lens Options
EDOF optics strive to extend the depth of focus, so that vision from distant to intermediate and close objects remains above a quality threshold. An EDOF has the advantage of replicating the pre-presbyopic state, in which accommodation naturally expands the depth of focus from distant to close.
One of only two commercially marketed EDOF contact lenses in the U.S. is the NaturalVue Multifocal 1 Day (Visioneering Technology) soft contact lens, which uses what the firm calls neurofocus optics.29 This one-of-a-kind design uses EDOF optics to deliver an “encompassing” add range of up to +3.00D.29 This is critical not only for presbyopes, but also for myopes.30,31 It’s a center-distance design, with increasing additional power traveling outward from the center.
The SynergEyes iD Multifocal EDOF is the second commercially available product (SynergEyes). A comparable layout was developed by researchers at the Brien Holden Vision Institute (BHVI).32-36 The BHVI design was compared to a center-distance, zonular design, which features a low and high add.32
In numerous respects, the optics of lenses with an EDOF differ from those of other commercially available soft multifocal designs. The distance and near power zones in a simultaneous view design are separate. Distant and near foci are established when a presbyopic eye is fitted with such a lens. Still, there is very little depth of focus, resulting in ghosting, reduced vision quality, lower contrast sensitivity, and undue influences of pupil size, centration, and illumination levels. The purpose of EDOF designs is to avoid the usual flaws in simultaneous view designs.32 When compared to the zonular design, its EDOF design performed better in the intermediate and near zones with no visual compromise at a distance.32
Previous designs have included aspheric or progressive power transitions and blending or stepping of the power profile to improve intermediate vision. However, these designs were limited by a shallow depth of field and cannot generate an EDOF with a high image quality from far to close.33 To increase focal depth, zonal designs with minimal central optic zones surrounded by enormous plus-power zones can generate “optical pinholes.” Nonetheless, their range of clear vision is limited.
EDOF designs that generate a natural extension of the depth of field have recently been developed.33 To extend the focus point, these designs combine numerous higher-order aberrations (HOAs) on the front surface of the lens.33 These lenses have distinct power profiles that set them apart from annular or aspheric versions with shallower focal depths. The power profile constantly changes by rapidly growing and receding (non-monotonically) across the optical zone (Figure 2).
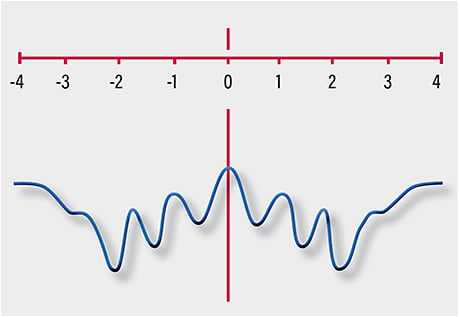
The EDOF in these lens designs would be expected to mitigate the visual impact of several factors, including individual aberrations of the eye, pupil size, and contact lens decentration.33 Also, power changes are very narrow and indiscrete (aperiodic)—not the broader square wave zones typically seen in annular designs. Thus, the non-monotonic and aperiodic power distribution from the combinations of HOAs (Zernike coefficients) delivers a more elongated depth of focus.33
In a study of 43 presbyopic individuals aged 42 to 66 years, subjects wearing EDOF lenses had a better visual performance at intermediate and near distances without decreasing distant vision.33 This study used a computer model for presbyopic emmetropes to evaluate anticipated outcomes for a through-focus design with low, medium, and high add powers, as well as center-distance, zonular, and center-near simultaneous views.33 The authors observed that EDOF designs are less vulnerable to pupil size variations, inherent ocular aberration, and decentration than concentric or simultaneous view designs.33 This finding was pursued in a prospective, participant-masked, randomized crossover trial using a variety of refractive errors and add powers.34 Each pair of lenses was worn for about a week. The results were consistent with those of two additional short-term comparisons of identical center-distance, zonular, and near-center, aspheric simultaneous vision designs worn daily.34-36 This study’s prototype had a slightly flatter base curve (8.5mm) and a bigger diameter (14.2mm) than the through-focus part 1 and part 2 studies.33,34 The combined findings from these studies suggest that EDOF presbyopia designs may have advantages over more popular center-near, simultaneous-view, and center-distance zonular designs.
Despite the weakness in research designs, the results are promising. EDOF optics are gaining in popularity, and their applications across various platforms offer some advantages over other designs. Time and improved research will tell how well EDOF lenses serve the larger population of presbyopes. For the moment, it’s good to have an alternative to provide our patients with the best possible contact lens care and worth your time to incorporate these developments in your presbyope clinical toolbox. ■
References
- Fricke T, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis, and modelling. Ophthalmol. 2018;125(10):1492-9.
- Vincent G, Velkoff V. The next four decades the older population in the United States: 2010 to 2050. Curr Pop Report. www.census.gov/prod/2010pubs/p25-1138.pdf . May 2010. Accessed March 11, 2019.
- Holden B, Fricke T, Wilson D, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmol. 2016;123(5):1036-42.
- Frick K, Joy S, Wilson D, et al. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmol. 2015;122(8):1706-10.
- Holden B, Fricke T, Ho S, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126(12):1731.
- Sade RM. The graying of America: challenges and controversies. J Law Med Ethics. 2012;40(1):6-9.
- Vargas-Fragoso V, Alió J. Corneal compensation of presbyopia: PresbyLASIK: an updated review. Eye Vis. 2017;4:11.
- Pallikaris I, Panagopoulou S. PresbyLASIK approach for the correction of presbyopia. Curr Opin Ophthalmol. 2015;26(4):265-72.
- Mosquera SA, Alió JL. Presbyopic correction on the cornea. Eye Vis. 2014;1:5.
- Luger M, McAlinden C, Buckhurst P, et al. Presbyopic LASIK using hybrid bi-aspheric micro-monovision ablation profile for presbyopic corneal treatments. Am J Ophthalmol. 2015;160(3):493-505.
- Schlote T, Heuberger A. Multifocal corneal ablation (Supracor) in hyperopic presbyopia: 1-year results in a cross-sectional study. Eur J Ophthalmol. 2017;27(4):438-42.
- Alio J, Plaza-Puche A, Férnandez-Buenaga R, et al. Multifocal intraocular lenses: An overview. Surv Ophthalmol. 2017;62(5):611–34.
- Chang D, Huggins L. Understanding the role of IOL optics in postoperative vision complaints. Rev Optom. 2018;155(12):48–51.
- Zvornicanin J, Zvornicanin E. Premium intraocular lenses: The past, present and future. J Curr Ophthalmol. 2018;30(4):267-96.
- Gundersen K. Rotational stability and visual performance 3 months after bilateral implantation of a new toric extended range of vision intraocular lens. Clin Ophthalmol. 2018;12(7):1269-78.
- Alió J, Simonov A, Romero D, et al. Analysis of accommodative performance of a new accommodative intraocular lens. J Refract Surg. 2018;34(2):78–83.
- Ong H, Evans J, Allan B. Accommodative intraocular lens versus standard monofocal intraocular lens implantation in cataract surgery. Cochrane Database Syst Rev. 2014 May 5;CD009667.
- Zhou H, Zhu C, Xu W, Zhou F. The efficacy of accommodative versus monofocal intraocular lenses for cataract patients. 2018;97(40): p e12693.
- Binder PS. Intracorneal inlays for the correction of presbyopia. Eye Contact Lens. 2017;43:267-75.
- Moarefi MA, Bafna S, Wiley W. A review of presbyopia treatment with corneal inlays. Ophthalmol Ther. 2017;6(1):55-65.
- Konstantopoulos A, Mehta JS. Surgical compensation of presbyopia with corneal inlays. Expert Rev Med Devices. 2015;12(3):341–52.
- Kleinmann G, Kim HJ, Yee RW. Scleral expansion procedure for the correction of presbyopia. Int Ophthalmol Clin 2006;46(3):1–12.
- Rex Ghormley N. The hydron ECHELON bifocal contact lens. Int Contact Lens Clin. 1989;16(4):315-7.
- Cole J. Can an eyedrop eliminate presbyopia? Rev Optom. 2017;154(6):42-6.
- Lombardo M, Lomabard G. Wave aberration of human eyes and new descriptors of image optical quality and visual performance. J Cat Refract Surg. 2010;36(2):313-31.
- Bruce A, Catania L. Clinical applications of wavefront refraction. Optom Vis Sci 2014;91(10):1278-86.
- Lawless M, Hodge C. Wavefront’s role in corneal refractive surgery. Clin Exp Ophthalmol. 2005;33(2):199-209.
- Appelgate R, Sarver E, Khemsara V. Are all aberrations equal? J Refract Surg 2002;18(5):S556-62.
- Visioneering Technology I. NaturalVue Multifocal Lens Specifications – Visioneering Technologies, Inc. Nat Multifocal Lens Specif 2018:1.
- Sankaridurg P. Contact lenses to slow progression of myopia. Clin Exp Optom. 2017;100(5):432-7.
- Cooper J, O’Connor B, Watanabe R, Fuerst R, Berger S, Eisenberg N, Dillehay SM. Case series analysis of myopic progression control with a unique extended depth of focus multifocal contact lens. Eye Contact Lens. 2018;44:e16–24.
- Tilia D, Bakaraju RC, Chung J, et al. Short-term visual performance of novel extended depth-of-focus contact lenses. Optom Vis Sci. 2016;93:435-44.
- Bakaraju RC, Ehrmann K, Ho A. Extended depth of focus contact lenses vs. two commercial multifocals: Part 1. Optical performance evaluation via computed through-focus retinal image quality metrics. J Optom. 2018;11:10–20.
- Bakaraju RC, Tilia D, Sha J, Diec J, Chung J, Kho D, Delaney S, Munro A, Thomas V. Extended depth of focus contact lenses vs. two commercial multifocals: Part 2. Visual performance after 1 week of lens wear. J Optom 2018;11:21–32.
- Tilia D, Munroa A, Chunga J, Shaa J, Delaney S, Khoa D, Thomas V, Ehrmanna K, Bakarajua RC. Short-term comparison between extended depth-of-focus prototype contact lenses and a commercially-available center-near multifocal. J Optom. 2017;10:14-25.
- Sha J, Tilia D, Kho D, Diec J, Thomas V, Bakaraju RC. Comparison of extended depth-of-focus prototype contact lenses With the 1-Day ACUVUE MOIST MULTIFOCAL after one week of wear. Eye Contact Lens. 2018;44:S157–63.









