Introduction
DIABETES IS A MULTISYSTEM disease of the body with ocular predicates and biomarkers that give eye care providers a unique opportunity to identify one of the most prevalent diseases of our time. As of 2021, nearly 537 million people worldwide were affected by diabetes with projections suggesting a rise to 643 million by 2030 and a staggering 784 million by 2045.1 Diabetes is a chronic metabolic disease characterized by elevated levels of glucose in the body and defects in insulin secretion, insulin function, or both.2 In this article, we review the effects of diabetes on accommodation and presbyopia.
Understanding Diabetes and Eye Health
Diabetes manifests as a continual elevation in blood glucose levels, often presenting alongside 3 hallmark symptoms: increased thirst (polydipsia), excessive hunger (polyphagia), and frequent urination (polyuria). It is categorized into 2 main types: type 1 and type 2.3 Type 1 diabetes mellitus is characterized by autoimmune destruction of the pancreatic beta-cells in the islets of Langerhans, resulting in absolute or near-total insulin deficiency. It is also known as insulin-dependent or juvenile-onset diabetes.
Conversely, type 2 diabetes mellitus or non-insulin-dependent diabetes mellitus has a higher incidence accounting for 80%–90% of all patients with diabetes. It involves mechanisms of insulin resistance, impaired insulin secretion, and inappropriate levels of circulating glucose, resulting in relative insulin deficiency. This type of diabetes may occur in genetically susceptible individuals with impaired insulin secretion or with insulin resistance and impaired regulation of glucose production in the liver.
Diabetes, characterized by chronic hyperglycemia, is associated with long-term damage, dysfunction, and failure of different organs, especially the eyes, kidneys, and nerves.4 In the eyes, it is implicated in myriad anterior- and posterior-segment disorders, of which the most commonly studied include diabetic retinopathy, diabetic cataract, refractive error, optic neuropathy, glaucoma, and ocular surface disorders. People with diabetes often experience blurred vision, a symptom largely attributed to changes in the refractive system of the eye.5
Ocular Manifestation of Diabetes: Diabetic Cataract
The clear crystalline lens is made up of elongated fiber cells containing high concentrations of crystallin proteins.6 There are 3 major types of crystallin present in the lens: α-, β-, and γ-crystallins.6 These proteins do not regenerate and therefore must last for our entire lifetime. The most common is α-crystallin, which acts as a chaperone for the other crystallins, binding to unfolded and damaged proteins before they can aggregate into complexes that cloud the lens. These chaperone crystallins do much of the work to keep the lens fibers organized, flexible, and clear.
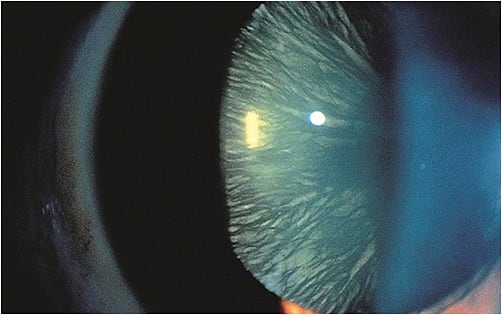
A cataract is defined as opacity within the clear, natural crystalline lens of the eye, which gradually results in vision deterioration. The literature suggests that the risk of developing cataracts increases with the duration of diabetes and poor metabolic control.7,8 Different types of cataracts can occur in diabetic patients, including cortical, nuclear, and posterior subcapsular cataracts. Cortical cataracts may occur independently of sugar level fluctuations, while posterior subcapsular cataracts are usually associated with poor glycemic control. Evidence suggests that cataracts develop earlier and more rapidly in diabetic patients.7,9 The Wisconsin Beaver Dam Study, the Australian Blue Mountains Eye Study, the Barbados Eye Study, the French Pathologies Oculaires Liées à l’Age Study, and the West African Countries (Ghana and Nigeria) Study collectively found that individuals with diabetes are up to 5 times more likely to develop cataracts.10-12
The pathogenesis of diabetic cataracts remains an area of ongoing study, lacking full comprehension despite numerous investigations. Thus far, sorbitol pathway hyperactivity, oxidative stress with the generation of reactive oxygen species (ROS), and the autophagy lysosomal pathway have been implicated in the development of diabetic cataracts.13
Sorbitol Pathway in Diabetic Cataract Pathogenesis
Diabetic cataracts involve heightened activity in the polyol pathway, leading to sorbitol accumulation within the lens.13 Elevated blood glucose levels in diabetes prompt the conversion of glucose into sorbitol via the enzyme aldose reductase. The buildup of sorbitol induces osmotic stress, altering lens hydration and contributing to cataract formation. This accumulation disrupts the normal function of lens proteins and enzymes, causing protein aggregation and lens opacification.
Oxidative Stress in Diabetic Cataract Pathogenesis
Oxidative stress significantly contributes to the onset of diabetic cataracts.13 Elevated blood glucose levels in diabetes trigger the production of ROS through various mechanisms, including the sorbitol pathway and the glycation of lens proteins. ROS accumulation damages lens proteins, lipids, and DNA, leading to opacification and cataract formation.
Autophagy-Lysosomal Pathway in Diabetic Cataract Pathogenesis
The autophagy-lysosomal pathway plays a role in the pathogenesis of diabetic cataracts.13 Autophagy is a cellular process that maintains homeostasis by degrading damaged or unnecessary cellular components. Impaired autophagy in the lenses of diabetic individuals leads to the accumulation of damaged proteins and organelles. This accumulation disrupts lens transparency and contributes to cataract development.
Impact of Uncontrolled Diabetes on Accommodation (Presbyopia)
The human eye can adjust its focus between distant and close objects by changing its dioptric power using a process known as accommodation. The crystalline lens in the eye, which is responsible for accommodation, can be affected by the changes induced by uncontrolled diabetes.14
One of the primary mechanisms contributing to impaired accommodation in diabetes involves the process of glycation. Elevated glucose levels in the bloodstream lead to increased formation of advanced glycation end-products (AGEs). These AGEs gradually accumulate within the lens proteins, causing crosslinking and structural modifications. As a result, the normally flexible and elastic properties of the crystalline lens become compromised. The lens loses its ability to change shape efficiently, thereby impeding the process of accommodation required for focusing on objects at different distances.
Furthermore, the osmotic changes induced by hyperglycemia play a crucial role in the pathophysiology of diabetic lens changes. The lens structure is highly dependent on its hydration levels for maintaining transparency and refractive properties. In diabetes, the elevated blood sugar levels create an osmotic gradient, leading to the increased influx of water into the lens. This influx disrupts the delicate balance of fluid within the lens, resulting in swelling and alterations in its refractive index. Consequently, these changes hinder the ability of the lens to alter its shape effectively during the accommodation process.
Another crucial factor contributing to the impaired accommodation in uncontrolled diabetes involves the impact of oxidative stress. The heightened oxidative stress resulting from prolonged hyperglycemia leads to the generation of free radicals and the depletion of antioxidant defense mechanisms within the lens. This oxidative insult causes damage to the structural integrity of the lens proteins, further exacerbating the loss of flexibility and compromising its accommodation capabilities.
This situation leads to a decrease in the amplitude of accommodation in persons with uncontrolled diabetes, as evidenced by the literature.15-17 People with uncontrolled diabetes are believed to become presbyopic at a younger age.18 Presbyopia is a physiological insufficiency of accommodation associated with the aging of the eye that results in progressively worsening ability to focus clearly on close objects.
Diagnostic and Management Strategies
Effective management of diabetes involves a range of treatment options aimed at controlling blood sugar levels and minimizing the risk of complications. Medications such as insulin, oral medications, and lifestyle adjustments play crucial roles. However, the impact of uncontrolled diabetes on vision extends beyond glucose control, often leading to ocular complications, such as diabetic cataracts, and a reduction in amplitude of accommodation, leading to early onset of presbyopia. These facts render acute refractive changes and presbyopia and lens glycation important biomarkers of diabetes.
Cataracts that develop as a result of alternative sorbitol pathway metabolism are often reversible, but on presentation they can result in an apparent resolution of presbyopia by improving the near point of vision, as impaired lens metabolism results in acute- or subacute-onset myopia. Identifying even subtle myopic shifts may be the result of diabetes in patients who may not otherwise know they have the condition. Concurrently, diabetes can disrupt accommodation, contributing to presbyopia, a condition effectively managed through glasses or contact lenses, which may reveal undiagnosed or poorly controlled systemic diabetes.
Prevention and early detection of diabetes are paramount to safeguarding against diabetic-related eye problems. Lifestyle modifications, such as a healthy diet, regular exercise, and weight control, are important discussions to have with all patients, but identification of ocular biomarkers, such as changes in refractive error, lens opacity, and early presbyopia, may lead to more timely education and intervention. For example, lenticular fluorescent glycation can be measured and has been shown to be highly sensitive and specific for diabetes.19 Technological advancements in this type of noninvasive lens imaging may ultimately improve early detection of diabetes during eye examinations.20 Currently, simple examination tools and diagnostics, such as refraction and slit-lamp exam of the lens, often reveal diabetes. The tools are ubiquitous in eyecare practices, further underscoring the importance of regular eye care for the global population.
Conclusion
In this review, we provide a comprehensive understanding of the relationship between uncontrolled diabetes and its ocular complications. Diabetes, whether type 1 or type 2, poses a significant risk to ocular health, leading to a spectrum of complications affecting the eye, including diabetic cataract and diminished accommodation.
The pathophysiological mechanisms involving heightened oxidative stress, alterations in the sorbitol pathway, and the impact on the autophagy-lysosomal pathway elucidate the mechanisms underlying diabetic cataract formation. Moreover, the interplay of glycation, osmotic changes, and oxidative stress significantly impairs the accommodation process, hastening the onset of presbyopia in individuals with diabetes.
Managing diabetes extends beyond glycemic control; it necessitates a comprehensive approach, including lifestyle modifications, routine eye examinations, and, when required, specialized interventions for ocular complications. Timely detection, preventive strategies, and a holistic approach to diabetes care are essential measures in mitigating the ocular sequelae associated with uncontrolled and undiagnosed diabetes.
As we navigate the rising global prevalence of diabetes, fostering awareness, advocating for regular screenings, and emphasizing the synergy between diabetes management and ocular health remain imperative in alleviating the burden of diabetic-related eye complications. The convergence of proactive management, innovative treatments, and preventive measures offers hope in preserving the vision and enhancing the quality of life of individuals living with diabetes. ■
References
- Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;36(Suppl 1):S67-S74.
- Forouhi NG, Wareham NJ. Epidemiology of diabetes. Medicine (Abingdon). 2019;47(1):22-27.
- Balaji R, Duraisamy R, Kumar MPS. Complications of diabetes mellitus: a review. Drug Invention Today. 2019;12(1):98-103.
- Kaštelan S, Gverović-Antunica A, Pelčić G, Gotovac M, Marković I, Kasun B. Refractive changes associated with diabetes mellitus. Semin Ophthalmol. 2018;33(7-8):838-845.
- Hejtmancik JF, Riazuddin SA, McGreal R, Liu W, Cvekl A, Shiels A. Lens biology and biochemistry. Prog Mol Biol Transl Sci. 2015;134:169-201.
- Pollreisz A, Schmidt-Erfurth U. Diabetic cataract: pathogenesis, epidemiology and treatment. J Ophthalmol. 2010;2010:608751.
- Drinkwater JJ, Davis WA, Davis TME. A systematic review of risk factors for cataract in type 2 diabetes. Diabetes Meta Res Rev. 2019;35(1):e3073.
- Obrosova IG, Chung SSM, Kador PF. Diabetic cataracts: mechanisms and management. Diabetes Meta Res Rev. 2010;26(3):172-180.
- Klein BEK, Klein R, Lee KE. Incidence of age-related cataract: the Beaver Dam Eye Study. Arch Ophthalmol. 1998;116(2):219-225.
- Mitchell P, Cumming RG, Attebo K, Panchapakesan J. Prevalence of cataract in Australia: the Blue Mountains Eye Study. Ophthalmology. 1997;104(4):581-588.
- Klein BEK, Klein R, Moss SE. Prevalence of cataracts in a population-based study of persons with diabetes mellitus. Ophthalmology. 1985;92(9):1191-1196.
- Mrugacz M, Pony-Uram M, Bryl A, Zorena K. Current approach to the pathogenesis of diabetic cataracts. Int J Mol Sci. 2023;24(7):6317.
- Donaldson PJ, Grey AC, Maceo Heilman B, Lim JC, Vaghefi E. The physiological optics of the lens. Prog Retin Eye Res. 2017;56:e1-e24.
- Adnan NE, Mathur A, Edwards K, Pritchard N, Suheimat M, Atchsion DA. Amplitude of accommodation in type 1 diabetes. Invest Ophthalmol Vis Sci. 2014;55(10):7014-7018.
- Moss SE, Klein R, Klein BE. Accommodative ability in younger-onset diabetes. Arch Ophthalmol. 1987;105(4):508-512.
- Mathebula SD, Makunyane PS. Amplitude of accommodation is reduced in pre-presbyopic diabetic patients. J Endocrinol Metab Diabetes S Afr. 2017;22(1):12-16.
- Khan A, Petropoulos IN, Ponirakis G, Malik RA. Visual complications in diabetes mellitus: beyond retinopathy. Diabet Med. 2017;34(4):478-484.
- Cahn F, Burd J, Ignotz K, Mishra S. Measurement of lens autofluorescence can distinguish subjects with diabetes from those without. J Diabetes Sci Technol. 2014;8(1):43-49.
- Zhang XM, Gao Y, Yang MX, et al. Exploration of noninvasive detection of advanced glycation end products in the lens to screen for diabetic kidney disease. Front Endocrinol (Lausanne). 2022;13:892070.