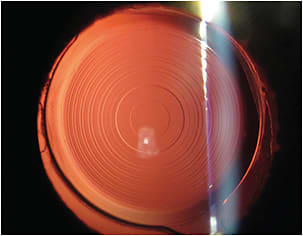
CATARACT SURGERY IS NOT only an opportunity to help patients see better but also an opportunity to tailor the intraocular lens (IOL) to minimize glasses dependence at distance or distance-intermediate-near. Presbyopia-correcting (PC)-IOLs have been around for more than 30 years, and like any technology, the improvements and innovations have led to greater levels of glasses independence, with a reduction in adverse events. Despite the improved IOL options for presbyopia, PC-IOLs have never cracked a 10% U.S. market share for cataract patients and have currently plateaued at around 7% over the last 5 years.1 Currently the most commonly implanted PC-IOL types are diffractive multifocal IOLs, diffractive trifocal IOLs, and extended depth of focus (EDOF) IOLs (both diffractive and nondiffractive) (Figure 1).
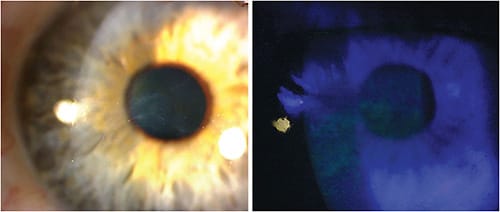
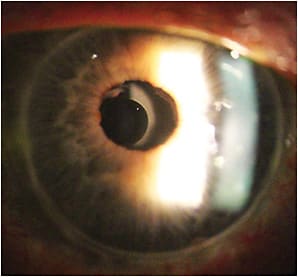
Preoperatively the IOL decision and conversation can be guided by 3 principles. First, listen and match the technology to the patients’ goals, not vice versa. Second, minimize other ocular pathologies and weigh this information heavily in the lens discussion. When appropriate, treat the pathology medically or surgically first (ie, reduce ocular surface disease before cataract surgery or perform a superficial keratectomy/phototherapeutic keratectomy in the presence of visually significant epithelial basement membrane dystrophy (Figure 2). In nonreversible pathologies (age-related macular degeneration, glaucoma with visual field loss, irregular astigmatism from keratoconus, or a corneal transplant), alter the optics to minimize negative aberrations and visual symptoms that could arise from diffractive IOLs (Figure 3). Finally, set the PC-IOL journey. For many patients, this can be 6-12 months for vision optimization. PC-IOLs are rarely “set it and forget it” scenarios.
Many PC-IOL patients are very happy when preoperative expectations are set correctly, but even in the best of hands, there will be the occasional disappointed patient. Here are 5 common postoperative concerns from patients that, with a targeted approach, can frequently be relieved or at least lessened.
1. “I CAN’T READ”: ADJUSTING TO A NEW NEAR POINT
Adjusting the near focal point is regularly an early postoperative adaptation in patients with a PC-IOL. Dependent on their preoperative habitual refractive error, many myopic patients will learn to push their reading materials slightly away. As a general rule, PC-IOLs will dedicate the majority of the incoming light energy to the distance foci, and a minority of light becomes focused for computer and near.2 Because of this tendency, intermediate and near vision can be augmented with supplementary lighting (ie, a tabletop reading lamp on the bedside nightstand). Extra light aids in pupil constriction, which increases depth of focus. Finally, regarding near vision, it is OK for patients to sporadically use over-the-counter readers/magnifiers, and I tell them this.
2. “EVERYTHING HAS RINGS, GLARE, AND HALOS”: POSITIVE DYSPHOTOPSIAS
In laymen’s terms, dysphotopsias are unwanted visual stimuli that result from incoming light that is off axis.2 Positive dysphotopsias are visual artifacts due to extra incoming light resulting in glare, starbursts, and halos.2 Listening closely to the type of dysphotopsia can elicit clues to the cause, and for diffractive PC-IOLs, “halos” are commonly associated with the inherent lens diffractive rings (Figure 4).2

According to a 2007 ASCRS/ESCRS survey, the number 1 cause of IOL explantation is disturbing glare/halos.3 A meta-analysis by Rosen et al reviewed survey studies that questioned cataract surgery patients about visual symptoms, and specific to disabling glare, it was reported at between 0% and 10% with diffractive multifocal IOLs (MFIOLs).4 There is a range for explantation rates in the literature due to glare/halo, but thankfully, the number is relatively low at 0.5% to 4% commonly.4,5
The good news regarding glare/halos/starburst is that time is our friend. Neuroplasticity refers to the brain’s ability to reorganize and adapt to a new environment in response to change.6 Rosa et al. performed a study of 45 participants (30 with a diffractive MFIOL and 15 with a monofocal IOL), in which they used functional MRI (fMRI) and quality of vision (QOV) questionnaires to study neuroadaptation at the 3-week and 6-month postoperative time points.6 In contrast to 3-weeks postoperatively, at the 6-month visit, fMRI did not show a significant difference or activation between the monofocal or MFIOL groups. Second, the MFIOL group showed a significant improvement in QOV score from the 3-week to 6-month surveys.6
3. “MY VISION FLUCTUATES A LOT, AND MY EYES BURN”: TEAR FILM INSTABILITY
Visual instability is a patient symptom that can frequently be attributed to underlying tear film deficiencies. There are many tools to aid in detection, such as tear osmolarity, inflammatory markers, meibography, noninvasive tear break-up time, and others, but patient visual symptoms can also point eyecare providers to dry eye. In the “frowning” PC-IOL patient, early in the postoperative period, managing providers should aggressively treat the ocular surface. Doing so not only has the potential to turn the frown upside down, but it also prepares the ocular surface for further refraction checks and/or corneal laser enhancements.
4. “MY VISION IS GETTING WORSE. ARE THE CATARACTS BACK?”: POSTERIOR CAPSULE OPACIFICATION
After the tear film has been optimized, closely examine the posterior capsule as a culprit for worsening vision or dysphotopsias in the PC-IOL patient. To avoid altering effective lens position (ELP), we prefer to wait at least 3 months before proceeding with an yttrium aluminum garnet (YAG) laser. A key reminder is that executing the YAG laser step is a 99% commitment to the implanted IOL because the posterior capsule is the key to a refractive IOL exchange. According to a Medicare data survey article, 36% of PC-IOLs had an ICD-10 diagnosis of posterior capsule opacification (PCO) less than 1 year postsurgery, but only 22% of these PC-IOL patients underwent YAG laser before 1 year.7 My experience is that roughly 50% of PC-IOL patients will undergo and benefit from YAG laser, so once you’re sure this IOL and this patient are a match, recommend this laser even in the presence of mild PCO. Yttrium laser to the posterior capsule is innocuous in most patients, with recent literature supporting the risk of retinal tear/detachment being 0.5% to 1%.8
5. “I’M STILL NOT SEEING AS WELL AS I HOPED I WOULD”: RESIDUAL REFRACTIVE ERROR
Now our patient has a pristine tear film and a well-positioned PC-IOL with an open capsule but residual refractive error. The phoropter and a detailed refraction will not only tell us the residual refractive error in diopters, but it will also home in on the patient’s image quality or crispness in vision with the appropriate refraction. Having an enhancement plan (LASIK, photorefractive keratectomy, astigmatic keratectomy) is essential in delighting in PC-IOL patients with even small amounts of refractive error. Uncorrected refractive error diminishes the IOL’s ability to deliver the intended optics. Generally, as the last step in the PC-IOL journey, if the refraction is stable and crisp, a corneal fine-tune will often get patients into the end zone.
For motivated patients, PC-IOLs can exceed patient expectations. With a thorough preoperative work-up and postoperative follow-up with the aforementioned steps, PC-IOLs not only can meet a patient’s goals but also can surpass them. When compared to monofocal IOLs, 2 independent studies have shown that MFIOLs performed near equally for uncorrected distance vision, but not surprisingly, MFIOLs performed significantly better at near.4 Teamwork in the PC-IOL journey leads to quoted satisfaction rates near 95% and spectacle independence rates exceeding 80% at all distances.4 In our practice, dependent on IOL technology, I have seen both of these percentages go even higher. ■
References
- US cataract quarterly update. Market Scope. Accessed April 21, 2023. https://www.market-scope.com/pages/reports/140/us-cataract-quarterly-update-q3-2019
- Thompson V. Optimization: The key to multifocal IOL success. Presbyopia Physician. 2023;3(1):17-21.
- Mamalis N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable intraocular lenses requiring explantation or secondary intervention–2007 survey update. J Cataract Refract Surg. 2008;34(9):1584-1591.
- Rosen E, Alio JL, Dick HB, Dell S, Slade S. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: Metaanalysis of peer-reviewed publications. J Cataract Refract Surg. 42(2):310-328.
- Venter JA, Barclay D, Pelouskova M, Bull CEL. Initial experience with a new refractive rotationally asymmetric multifocal intraocular lens. J Refract Surg. 2014;30(11):770-776.
- Rosa AM, Miranda AC, Patricio MM, et al. Functional magnetic resonance imaging to assess neuroadaptation to multifocal intraocular lenses. J Cataract Refract Surg. 2017;43(10):1287-1296.
- Terveen D, Berdahl J, Dhariwal M, Meng Q. Real-world cataract surgery complications and secondary interventions incidence rates: an analysis of US Medicare claims database. J Ophthalmol. 2022;2022:8653476.
- Wesolosky JD, Tennant M, Rudnisky CJ. Rate of retinal tear and detachment after neodymium:YAG capsulotomy. J Cataract Refract Surg. 2017;43(7):923-928.









