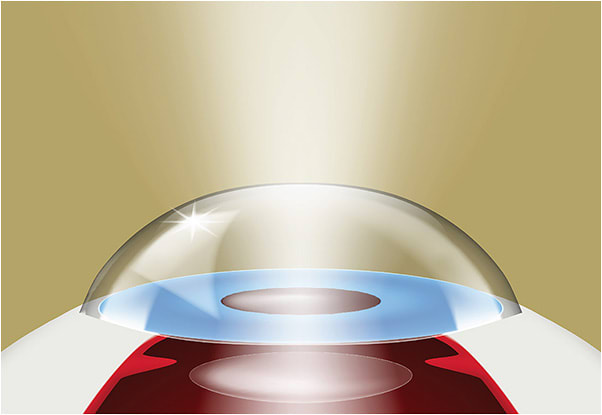
THE INTRODUCTION OF THE Light Adjustable Lens (LAL) has led to a paradigm shift in cataract surgery. With traditional surgery, postoperative refractive precision is dependent on preoperative biometry. Modern formulas consider a number of variables in an attempt to predict the intraocular lens (IOL) power needed to achieve a desired refractive outcome; unfortunately, even the most advanced formulas are unable to account for individual healing processes and resultant effective lens position (ELP). The expectations of the average cataract patient have evolved as much as the procedure itself in the last few decades, in part due to the proven success of corneal refractive procedures. Gone are the days of thick glasses after surgery—full, uncompromised spectacle independence is now the premium outcome our patients want.
Setting the Stage: 20/Happy
Patient perception is as important as surgical outcome in reality. The buffet of IOL options can be overwhelming for patients. The discussion about which option is best revolves around a hypothetical world, ie, a world without a cataract impacting visual quality. The LAL allows much of this discussion to happen well after surgery, giving the patient a comforting feeling of control. After the cataract is removed, patients are able to better understand how a certain refractive condition will impact their lifestyle. They can then “test drive” and adjust their target on the fly to match their lifestyle needs. It has been suggested that eye dominance changes in roughly 20% of patients following cataract surgery.1 Determining eye dominance is important for refractive targeting. Understanding that this may change in a patient postoperatively, it’s easy to see why having refractive discussions after surgery would be advantageous.
The LAL isn’t for the impatient patient. There is a substantial logistical burden that must be outlined. After the lenses are implanted in the typical fashion, at least 2 weeks must pass to allow for refractive stability before the first light adjustment can take place. Patients may need up to 3 adjustments, followed by 2 mandatory lock-in visits, with each of these encounters separated by 3 days. Additionally, because ultraviolet light (UV) is used to induce refractive change during the light adjustment procedures, patients are required to wear the provided UV protective glasses while outdoors or in high UV exposure settings prior to final lock-in. On average, patients can expect the process from surgery to final lock to take about 4-6 weeks.
I view the light adjustments as similar to a contact lens fit. I use trial frames and loose lenses to simulate an outcome, taking feedback from the patient to set a target. Patients then test drive their vision for at least 3 days before returning for their next adjustment. ActivShield (RxSight), an added UV protective coating to the anterior surface of the LAL, was introduced in 2021. Since its introduction, we have seen a higher degree of accuracy in our practice while no longer requiring patients to wear their UV glasses indoors.
The Monofocal IOL With a Twist
A misconception about the LAL is that it’s a simple monofocal lens aimed at precision distance vision. While this is partly true, it’s also highly oversimplified. It is indeed a monofocal lens; however, given its aspheric design, it does allow for an element of extended depth of focus (EDOF). This aids in extending visual range even in a plano targeted eye. Additionally, patients can elect to add negative spherical aberration to their nondominant eye during the light treatments. This adds an additional 0.50D-0.75D of EDOF, providing a solution for presbyopia and reducing the need for reading glasses postoperatively. In our practice, we have strayed away from the term “monovision” as it implies full ocular independence and loss of binocular balance. Instead, we use the term “blended vision” because there is substantial overlap between the eyes, allowing for binocular summation for maintained depth perception. About 80% of our patients choose some form of blended vision, with the nondominant target being -1.00D to 1.25D on average. The beauty of the LAL is that we can customize the near target based on lifestyle. The added EDOF of the nondominant eye still preserves usable distance visual acuity. Even with a -1.25D target, a healthy patient can often maintain 20/30 or better unaided distance visual acuity without glare or halos.
The LAL has a spherical range of +/- 2.00D sphere and up to -3.00D cylinder.2 Because of its cylindrical range, postoperative stability, and customization potential, we use the LAL far more often than monofocal toric IOLs in astigmatic patients.
The Perfect Patient
As all refractive surgeons know, refractive precision is more elusive in a post-LASIK patient. The alteration of corneal architecture results in a miscalculated ELP, which in turn can lead to a refractive surprise. Post-LASIK patients commonly have lower tolerance for refractive error because of their years of spectacle independence. The LAL is a perfect solution for these patients, delivering LASIK-type results consistently. The LAL provides outcomes within 0.50D 92.1% of the time at 6 months postop according to the 2017 FDA trial, which is similar to modern corneal refractive procedures.3 Compare this with a roughly 72% success rate with monofocal IOLs.4 We have seen similar, if not better, results in our practice with the second-generation LAL with ActivShield.
While the post-LASIK patient seems like a slam dunk, we have repeated success with patients of all types, including those with active corneal or retinal pathology and even severe glaucoma. While other multifocal or EDOF IOLs require pristine corneal and retinal health due to their optical nature, the LAL is a monofocal lens that is not influenced by subtle corneal or retinal irregularities. Unlike multifocal IOLs, it is reasonable to offer the LAL to patients with age-related macular degeneration, an epiretinal membrane, or glaucoma. While the optional added negative spherical aberration to induce EDOF may not always be in the patient’s best interest, the ability for monofocal refractive precision is something from which all patients can benefit. We have experienced overwhelming success with post-radial keratotomy patients as well as with younger pre-presbyopic patients.
Pearls for Success
It’s no secret that the LAL comes with its share of challenges.
- Detailed discussion is essential prior to surgery. I often speak in analogies to help the patient understand the process. They must understand that this is a marathon, not a sprint. Similar to tailoring a fine tuxedo, it takes time, but the results will be custom and precise. As another analogy, I liken traditional cataract surgery to a par 3 on a golf course but only allowing a single swing—getting the ball on the green is a decent shot, and usually we’re satisfied with that. With the LAL, we now get the chance to putt it 3 times, and are expecting to get it in the hole.
- The surgical target should be set for plano with both eyes regardless of the final refractive target. This allows for re-establishment of eye dominance postoperatively and allows room for the added negative spherical aberration to enhance depth of focus in the nondominant eye.
- Tear film maintenance prior to surgery is key with the LAL, as it is for all refractive surgeries. The tear film will drive the refraction, which is the dependent variable that we’re trying to control. All of our patients are on a regimen of preservative-free artificial tears and lid hygiene beginning at the very least 2 weeks before surgery and continuing throughout the entire adjustment process. The light adjustments will often disrupt the tear film further, so starting prophylactic maintenance therapy is always advisable. Along the same lines, having the same clinician perform the subjective refractions is important to ensure reliability and repeatability.
- Staff education is arguably as important as patient education. There will be multiple visits for these patients—needless to say, our staff will get to know them quite well during their light adjustment process. We ask our staff to engage with each patient and celebrate steps of improvement along the way. The day of the final lock-in is graduation, signifying the end of a long journey. We make sure to celebrate that with our patients, and they truly appreciate the team approach.
Conclusion
The LAL is arguably the largest technological advancement in cataract surgery in recent decades. As a monofocal lens, it has applications in patients with significant ocular disease. The ability to customize range of vision further distances patients from spectacle dependence without inducing glare or halos as with multifocal IOLs—a giant leap toward the elusive cataract surgery holy grail. ■
References
- Schwartz R, Yatziv Y. The effect of cataract surgery on ocular dominance. Clin Ophthalmol. 2015;9:2329-2333
- Walton OB. Adjusting to the Light Adjustable Lens. Ophthalmol Mgmt. 2021;25(2):36,38,41.
- US Food and Drug Administration. News Release. FDA approves first implanted lens that can be adjusted after cataract surgery to improve vision without eyeglasses in some patients. 2017 November 22. https://www.fda.gov/news-events/press-announcements/fda-approves-first-implanted-lens-can-be-adjusted-after-cataract-surgery-improve-vision-without
- Lundstrom M, Dickman M, Henry Y, et al. Risk factors for refractive error after cataract surgery: Analysis of 282 811 cataract extractions reported to the European Registry of Quality Outcomes for cataract and refractive surgery. J Refract Cataract Surg. 2018; 44(4):447-452.









