Introduction
A PRIMARY FOCUS IN OPHTHALMIC health care has been on providing solutions to help our patients “see” more clearly and curtail the effects of uncurable age-related eye diseases, such as presbyopia, cataracts, glaucoma, and age-related macular degeneration (AMD). The eye contains more than 2 million working parts and is considered the second most complex organ in the body next only to the brain.1 Considering that the muscles of the eye are the fastest and strongest in the body with a resilient capability to adjust to rapidly changing conditions, it is surprising that more in-depth neuromuscular and biomechanical constructs have not been a fundamental cornerstone of ophthalmic education.2 Nonetheless, a more extensive understanding of the physiological and biomechanical mechanisms is essential to developing more anatomically congruous innovations for treatment solutions, as well as disease prevention.
We do not often think of the eye in biomechanical terms, instead relegating it to a mere light-transducing optical organ. However, the eye is an intricate biomechanical machine: it is a pressurized sensing device capable of whole organ and precise intraorgan movements, as well as complex biotransport and elegant hydrodynamic drainage systems, all driven by extraocular and intraocular neuromuscular engines.3,4 When discussing the dynamic functions of the eye, it is of critical importance to understand the structure and function of its elaborate design and, most specifically, the biomechanical mechanisms that are cardinal for the efficient function of the eye organ, both visually and physiologically.
Outlined in Figure 1 below are the key anatomical components that all have unique structures and functions that contribute to the efficient Dynamic Range of Focus (DRoF) capability of the eye for a given visual task, which is both a necessary and a precise biomechanical function that allows the eye to process visual information with the best focus possible given a particular visual system.
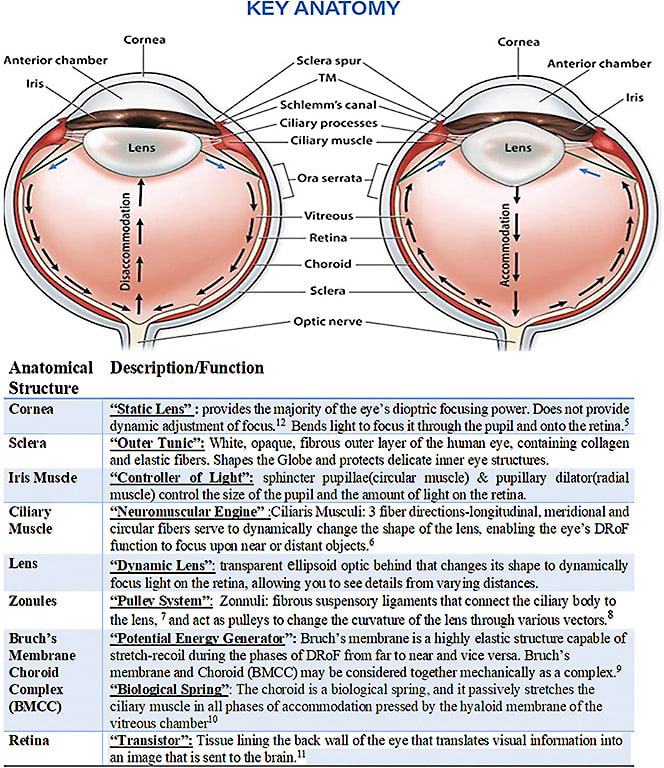
Given this complexity, biomechanics can be the key to understanding the normal functions involved in dynamic accommodation—dynamic focusing between phases of near-to-far and far-to-near—as well as other intricate physiological processes of the eye, such as the regulation of intraocular pressure, aqueous outflow dynamics, and circulation of ocular blood flow. In addition, understanding the pathogenesis of common disorders, such as presbyopia, glaucoma, AMD, and myopia, is enabled when we take a biomechanical view, rather than viewing the eye as simply an “optic.”14-21 In this review, we give an overview of ocular biomechanics and the critical importance of the dynamic internal movements of the eye, namely the eye’s ability to perform DRoF with concentration on the impact of biomechanics and kinematics. We further emphasize the understanding of the dynamic mechanical events occurring inside of the eye organ necessary to perform highly complex and efficient tasks as a response to numerous neuromuscular commands.
Ocular Biomechanics
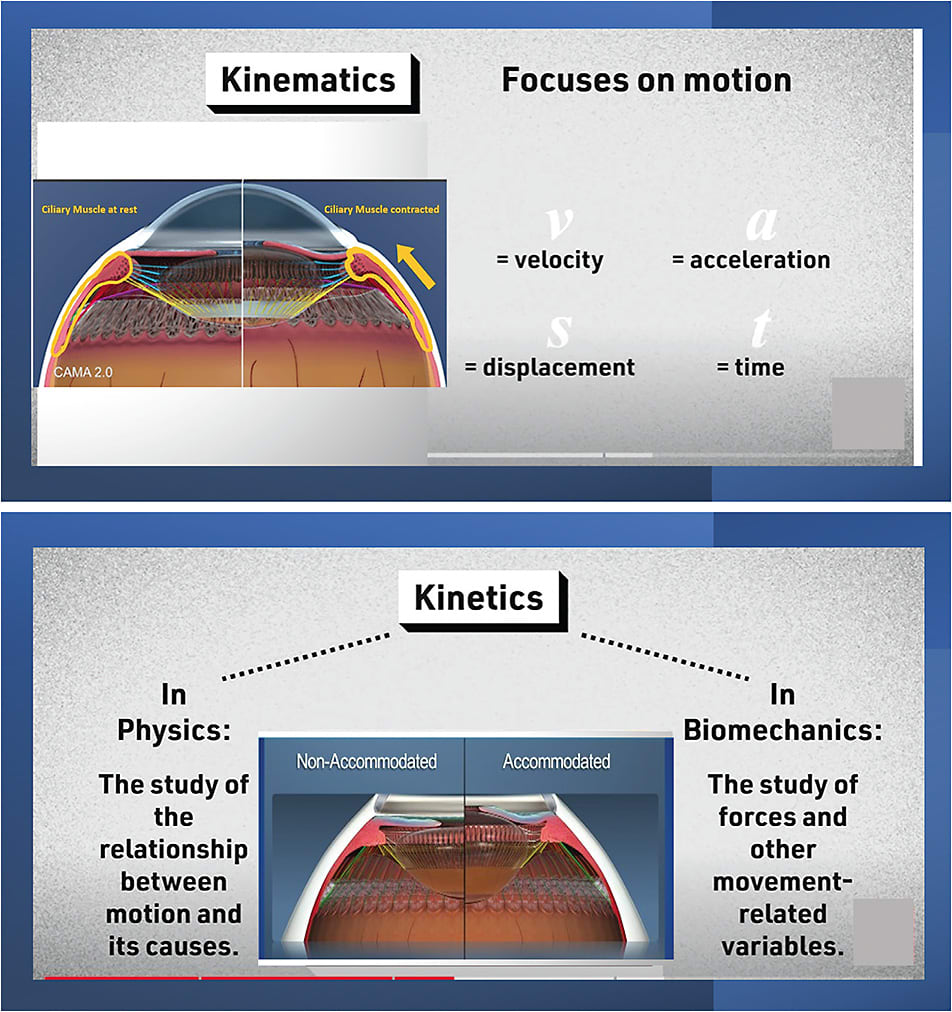
Biomechanics is the study of human movement, by which all moving structures can be analyzed. Biomechanical principles must be considered in the examination of the internal and external forces that produce or control movement and to understand structure and function of muscle movements and the impact of forces on connective tissues, muscles, capsules, and other related anatomic structures.22 Biomechanics can be broken down into 2 broad areas: statics and dynamics. Statics include geometry and stress, which fall under the mechanical laws of physics, while dynamics is broken down into kinetics and kinematics. Kinetics is the study of forces acting on “rigid bodies,” and kinematics describes the mechanics of body movements without considering the forces that cause them to move (Figure 2).23

Ocular biomechanics is not a new field. In fact, it is a primary point of interest in the posterior globe due to its effects on the pathophysiology of age-related diseases, such as glaucoma and AMD.24-26 By contrast, the study of ocular biomechanics in the anterior globe as it relates to the effects on pathophysiology of age-related diseases affecting the anterior segment, such as presbyopia and open angle glaucoma, has been sparse. Nonetheless, the development of ocular biomechanics and kinematics constructs in the anterior globe for translation into clinical utility is a promising area of study.15,17,20,21,27 The process of DRoF, accommodation and disaccommodation belongs squarely in the fields of biomechanics and kinematics because it involves movement and related forces.
It is of critical importance to understand the kinematics, or the behavior of the accommodative/disaccommodative movements or the geometry of motion; related displacement, velocity, acceleration, and time, without reference to the cause of the motion during dynamic focusing. Moreover, we must also understand the kinetics of dynamic focusing in order to have a way to explicate the forces occurring during accommodation/disaccommodation as well as other movement-related variables involved in the function of DRoF (Figure 3).
Accommodative/disaccommodative movements involve complex interactions of muscle function and joint lever systems under the control of the nervous system: the ciliary ganglion and ultimately the master and commander—the brain. When studying dynamic neuromuscular movements like those of the musculi ciliaris (ciliary muscles) of the eye, it is important to fully comprehend the mechanical and physical laws that govern these movements, as well as the biomechanical interactions between the anatomical structures in the eye. Although it is almost impossible to capture all of the biomechanical aspects that contribute to DRoF function, we provide here an overview of major components of this complex biomechanical apparatus.
Conclusion
Ocular biomechanics are fundamental to the basic functioning of the eye and its ability to adjust focus dynamically. Since this capability is inherent to how the eye “works” naturally, there must be an effort to push forward the knowledge of biomechanics in the anterior segment. This would further develop the opportunities for treatment solutions and interventions that are recovery based and not simply vision correction based. Rehabilitation is currently proven to be an effective intervention for recovery of function in other areas of the body where biomechanical issues involving muscles, ligaments, and capsules exist. Likewise, rehabilitation for vision recovery given the proper identification and solutions for a specific biomechanical dysfunction in the eye organ is possible.29 The eye organ, by design, is inherently built to perform enormously complex and intelligent biomechanical movements based on neural commands from our consciousness that enable our communication with the visual experiences that we enjoy from the moment we open our eyes. This makes vision the most precious and miraculous experience we take for granted every day. Our fundamental understanding of the intricate movements that produce function in the eye organ is void of comprehension regarding the impact of biomechanics and kinematics. At best, we posess an incomplete understanding of the application of mechanical laws of physics to DRoF functionality and the biomchanical behavior of accommodative structures in both phakic and pseudophakic eyes. This gap in our knowledge has retarded our ability to create viable and sustainable technology intervention in the anterior segment specifically to address presbyopia and glaucoma.
This is Part I in a series of articles that will serve as a deeper dive into ocular biomechanics in the hope of bringing a new awareness to dynamic mechanisms occurring in the eye as a response to all of the visual commands which require dynamic focusing mchanisms. A much needed paradigm shift of adding biomechanical applications to solving dynamic problems in the eye organ is essential in finding more sustainable treatment solutions for age-related eye diseases that impact our visual dynamic functions. Since the presbyopia market of 2.1 billion people globally reemains a significant unmet and growing market, it is vital that we gain further knowledge in this area.30
We will continue to explore the kinematics of DRoF by illuminating the executive mechanisms involved as well as outlining the “phases of DRoF” specific to the biomechanical interrelationships in the next issue! Stay tuned... ■
References
- How does the eye work? Optometrists.org . Published October 11, 2020. Accessed February 17, 2023. https://www.optometrists.org/general-practice-optometry/guide-to-eye-health/how-does-the-eye-work/
- Croft MA, Glasser A, Kaufman PL. Accommodation and presbyopia. Int Ophthalmol Clin. 2001;41(2):33-46.
- Ethier CR, Johnson M, Ruberti J. Ocular biomechanics and biotransport. Annu Rev Biomed Eng. 2004;6:249-273.
- Croft MA, Kaufman PL. Accommodation and presbyopia: the ciliary neuromuscular view. Ophthalmol Clin North Am. 2006;19(1):13-24.
- Hejtmancik JF, Shiels A. Overview of the lens. Prog Mol Biol Transl Sci. 2015;134:119-127.
- Glasser A. Accommodation. In: Dartt DA, ed. Encyclopedia of the Eye. Academic Press; 2010:8-17.
- Wikipedia contributors. Zonule of Zinn. Wikipedia, The Free Encyclopedia. Published January 22, 2023. Accessed February 19, 2012. https://en.wikipedia.org/w/index.php?title=Zonule_of_Zinn&oldid=1135127804
- Nankivil D, Maceo Heilman B, Durkee H, et al. The zonules selectively alter the shape of the lens during accommodation based on the location of their anchorage points. Invest Ophthalmol Vis Sci. 2015;56(3):1751-1760.
- Ugarte M, Hussain AA, Marshall J. An experimental study of the elastic properties of the human Bruch’s membrane-choroid complex: relevance to ageing. Br J Ophthalmol. 2006;90(5):621-626.
- Koshits IN, Svetlova OV, Egemberdiev MB, Guseva MG, Markarov FN, Roselo Kesada NM. Theory: Morphological and functional features of the structure of the zonula lens fibers as a key executive link in the mechanism of the human eye accommodation. J Clin Res Ophthalmol. 2020;7:61-74.
- Nguyen KH, Patel BC, Tadi P. Anatomy, Head and Neck, Eye Retina. StatPearls Publishing; 2022.
- Optical properties of the eye. American Academy of Ophthalmology. Accessed February 16, 2023. https://www.aao.org/munnerlyn-laser-surgery-center/optical-properties-of-eye
- Kaufman PL, Lütjen Drecoll E, Croft MA. Presbyopia and Glaucoma: Two Diseases, One Pathophysiology? The 2017 Friedenwald Lecture. Invest Ophthalmol Vis Sci. 2019;60(5):1801-1812.
- Martin H, Stachs O, Guthoff R, Grabow N, Jünemann A. Biomechanische Untersuchungen zur Akkommodation des Auges. Ophthalmologe. 2018;115(8):649-654.
- Hipsley A, Colbert M. The zooming eye lens: effects of age on dynamic range of focus. Presbyopia Physician. September 2022:32-36.
- Hipsley AM, Dementiev D. VisioDynamics Theory A Biomechanical Model for the Aging Ocular Organ. Jaypee Brothers Medical Publishers; 2006.
- Ting DSJ, Liu YC, Price ER, et al. Improvement in accommodation and dynamic range of focus after laser scleral microporation: a potential treatment for presbyopia. Transl Vis Sci Technol. 2022;11(12):2.
- Swartz TS, Rocha KM, Jackson M, Ma DHK, Goldberg D, Hipsley A. Restoration of accommodation: new perspectives. Arq Bras Oftalmol. 2014;77(1):V-VII.
- Hipsley AM, Hall B. Influence of ocular rigidity and ocular biomechanics on the pathogenesis of age-related presbyopia. In: Pallikaris I, Tsilimbaris MK, Dastiridou AL, eds. Ocular Rigidity, Biomechanics and Hydrodynamics of the Eye. Springer, Cham; 2021:127-146.
- Hipsley A, Price ER. Ocular health implications of the loss of dynamic range of focus function in presbyopia. Presbyopia Physician. 2022;2:26-29.
- Girard MJA, Dupps WJ, Baskaran M, et al. Translating ocular biomechanics into clinical practice: current state and future prospects. Curr Eye Res. 2015;40(1):1-18.
- Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. F.A. Davis; 2011.
- Kinematics and dynamics in special relativity. MathPages. Accessed February 13, 2023. https://www.mathpages.com/home/kmath692/kmath692.htm
- Sigal IA, Roberts MD, Girard M, Burgoyne CF, Downs JC. Biomechanical changes of the optic disc. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Elsevier/Saunders; 2010:153-164.
- Fazio MA, Grytz R, Morris JS, Bruno L, Girkin CA, Downs JC. Human scleral structural stiffness increases more rapidly with age in donors of African descent compared to donors of European descent. Invest Ophthalmol Vis Sci. 2014;55(11):7189-7198.
- Fazio MA, Grytz R, Bruno L, et al. Regional variations in mechanical strain in the posterior human sclera. Invest Ophthalmol Vis Sci. 2012;53(9):5326-5333.
- Knaus KR, Hipsley A, Blemker SS. The action of ciliary muscle contraction on accommodation of the lens explored with a 3D model. Biomech Model Mechanobiol. 2021;20(3):879-894.
- Goldberg DB. Computer-animated model of accommodation and presbyopia. J Cataract Refract Surg. 2015;41(2):437-445.
- Maxey L, Magnusson J. Rehabilitation for the Postsurgical Orthopedic Patient. Elsevier Health Sciences; 2013.
- Presbyopia Physician - Presbyopia by the Numbers: Who Is Affected by It? Presbyopia Physician, Volume: 2, Issue: June 2022, page(s): 24-26. Accessed February 17, 2023. https://www.presbyopiaphysician.com/issues/2022/june-2022/presbyopia-by-the-numbers-who-is-affected-by-it











