Guest authors
John A. Hovanesian, MDShayna Mellesmoen, OD
Jessica Heckman, OD
Y. Ralph Chu, MD
CASE REPORT
A 60-year-old man presents for cataract consultation. He has a history of myopic LASIK OU performed in 1999 and wants to have the best range of vision without glasses as much as possible after surgery.
- BCVA OD: 20/25-1; BCVA OS 20/20
- MRX OD: +0.50+1.50x 011 20/20 Glare 20/400
- MRX OS: +0.50+0.75x 173 20/20 Glare 20/400
- SLE:
- - LL: mild blepharitis OU
- - C/S: white, quiet
- - K: +LASIK flap OU
- - a/c: d/w OU
- - Iris: r/r OU
- - Lens: 1+ NS OU
- DFE: wnl OU
JOHN A. HOVANESIAN, MDHarvard Eye Associates, Laguna Hills, CA
IN MANY WAYS, THESE PATIENTS ARE THE TOUGHEST ones we treat. Presbyopia patients with plano refractive error who have undergone LASIK and have near emmetropia, but not severe enough cataracts to cause disabling symptoms.
At age 60, many patients continue to drive after dark regularly and have high visual demands in both their occupational and spare time activities. The therapeutic options are few: presbyopia drops, LASIK or photorefractive keratotomy, and refractive lensectomy.
Presbyopia drops, pending a proper retina exam for high axial myopia and proper counseling on side effects, could be an important first step. The miotic effect might mitigate the residual astigmatism’s effect on distance vision while providing better near range of focus. I would be guarded in promising too much from presbyopia drops, however. Patients older than 60 with early cataracts usually have limited results from Vuity (pilocarpine hydrochloride ophthalmic solution, Allergan), which is the only available product at this time.
Another nonsurgical step that might make sense for this patient is to try monovision with contact lenses. Doing so would establish his comfort with this unique approach, which would offer a number of promising possibilities.
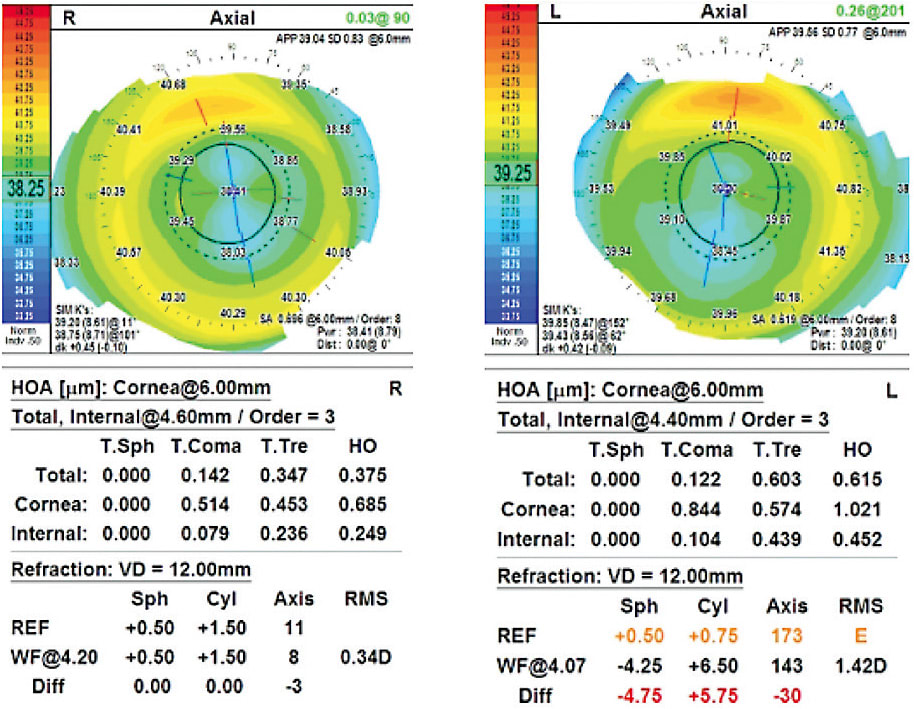
Keratorefractive solutions probably should be avoided because the patient already has a moderate amount of higher-order aberrations, which would likely become worse. Laser treatment would likely worsen the ocular surface disease as well, and the refractive results are not ideal for patients who had LASIK long ago because of irregular epithelial thickening.
Lens-based surgery, such as refractive lensectomy, probably makes the most sense because this patient, at age 60, likely has little remaining accommodation, and his crystalline lenses are, if anything, degrading rather than contributing to good clarity. This patient could do very well with an Apthera (formerly IC-8) small-aperture implant (AcuFocus and Bausch + Lomb) because of this lens’s unique ability to remedy astigmatism, neutralize higher-order aberrations, and generate a satisfactory range of focus. Assuming the patient was receptive to monovision, I would treat the nondominant eye first, targeting -0.75. Then, after surgery, the patient could assess whether the same lens could be used with a distance target in his dominant eye. The patient would need to be willing to accept a mild degree of visual dimming, which this lens causes in some patients.
A nondiffractive extended depth of focus (EDOF) lens like Vivity (Alcon), again targeting mini-monovision, or a diffractive EDOF lens like Synergy (Johnson & Johnson Vision) would be other options, with the advantages of simplicity in planning and excellent astigmatism correction.
Finally, my choice for this patient would probably be the light-adjustable lens (LAL, RxSight). This lens can easily correct the patient’s astigmatism and be set for plano and -0.75, which surprisingly gives most patients a full range of vision binocularly. Most importantly, the LAL achieves better precision of correction than any other lens option. Psychologically, patients who undergo the adjustments inherent in LAL correction have personal “ownership” of their visual outcomes because they participated in the final outcome by wearing the ultraviolet (UV)-protecting spectacles and returned for additional visits. They tend to be the happiest patients of all.
Regardless of which lens is chosen, it would be important to ensure the proper intraocular lens (IOL) calculations are done. This patient has long, 26+ mm eyes and flat corneas after LASIK with average keratometry values of about 38 D. It would be important to use advanced generation formulas, like the Barrett True K, and to correct the error on the biometry printout, where it appears that the patient has been entered as “no postrefractive,” as this might cause confusion.
Most importantly, this type of patient needs to be educated that all approaches will fail to provide perfect vision because of the limitations of the previously altered cornea. I like to show patients their own topography, explaining how the variations in color represent visual irregularities that cannot be corrected by any current technology. While LASIK served an important purpose in this patient’s life for more than 25 years, the residual irregularity is a minor liability. ■
SHAYNA MELLESMOEN, OD, JESSICA HECKMAN, OD, AND Y. RALPH CHU, MDChu Vision Institute, Bloomington, MN
THIS PATIENT IS A GREAT EXAMPLE OF A VERY FREQUENTLY seen clinical case in our practice. LASIK has been approved for more than 20 years. As a result, increasing numbers of patients with a history of refractive surgery are presenting for cataract surgery and looking for a great refractive outcome, as is the case for this patient.
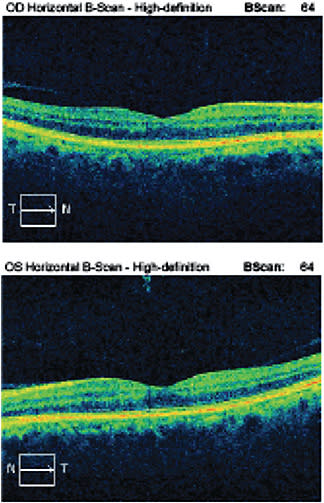
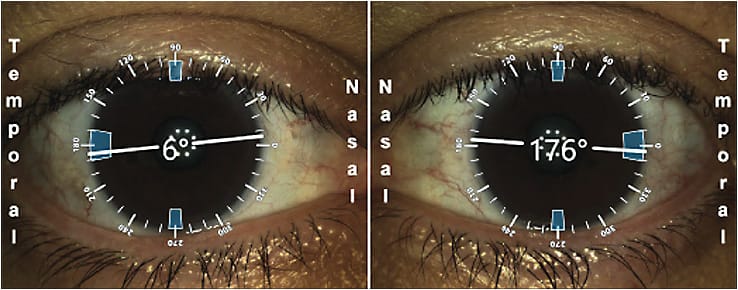
This patient’s topography indicates he underwent previous myopic LASIK. The keratometry values and axial length suggest that it likely was not an extremely high degree of myopia that was corrected with his refractive procedure. The topographic pattern appears to be regular without signs of ectasia or significant irregularity. Optical coherence tomography of the patient’s maculas appears to be clear of pathology. In addition, the biometry data show px and py at values where the centration of an IOL over the patient’s visual axis is likely.
Given this patient’s desire for least dependency on glasses, a trifocal IOL could be considered. The regular topographic pattern without overly flat keratometry values is a corneal attribute representative of the postrefractive patients in whom we have found success with a multifocal or trifocal type of lens. This patient also has a healthy macula, and the implant is likely to center over the visual axis, which are important factors for the patient to have the best visual outcome with this type of lens. While the trifocal lens offers the promise of reduced dependency on glasses, its success is highly dependent on the refractive outcome postoperatively. Given the potential for inaccuracy in cataract surgery with postrefractive corneas, it is also important to consider whether the patient could have a laser vision correction enhancement in the case of a refractive surprise. Given the data presented in this case, it seems to be an appropriate consideration should this patient be in that situation postoperatively.
The LAL is the other lens that we would consider for this patient. The ability to adjust the refractive outcome of a patient after implantation using UV light exposure has been invaluable for the postrefractive patient. It allows for a planned adjustment to target the patient’s most functional vision after surgical healing has stabilized vs the need for the patient to undergo a secondary laser vision correction enhancement procedure. This particular patient does not appear to have a history of monovision so would be targeted for distance in both eyes with the expectation to use near glasses after surgery. However, in our experience, the asphericity of the LAL does seem to allow for a broader range of focus than a traditional monofocal IOL. Additionally, many patients tend to tolerate a mild degree of monovision to allow for larger ranges of focus with this lens technology, which can be adjusted depending on the patient’s tolerance.
Fortunately, this patient has ocular characteristics that allow for great options of IOLs for his cataract surgery. Given the increased accuracy from the planned adjustability of the LAL, it would be our top choice for this patient.
Dr. Loh’s Approach
Prior to surgery, we discussed multiple IOL options, and I stressed that, due to the history of prior myopic LASIK and increased higher-order aberrations in the left eye, there was an increased risk of a postoperative refractive surprise. In addition, the presence of higher-order aberrations could impact the success with a multifocal IOL and not provide satisfactory quality of vision. Luckily, the patient had a healthy retinal exam and normal foveal contour. I recommended the RXSight LAL, with the intention of correcting his astigmatism and creating a mini-monovision to give him more range of vision. Due to the postoperative adjustability of the LAL, there is also an increased chance to achieve the intended refractive target.
The patient underwent femtosecond laser-assisted cataract surgery on his right eye and, 1 week later, on his left eye. His initial target for both eyes was plano, with the intent to induce myopia in one eye. I was thankful that the patient chose the LAL because his OD ended up with a -1.25+1.75x 010 refraction in the immediate postop period (targeted for plano).
After several weeks of healing, the light adjustment treatments were started. His right eye was treated to a -1.25 sphericity refraction, and he was able to see with uncorrected visual acuity of 20/20-2 and J1+ near. He was thrilled with his right eye. His left eye (which was planned to be targeted for distance) developed an early-onset posterior capsular opacity between the second and third light treatments and could not be refracted to 20/20 as a result. A YAG capsulotomy was performed, and the third light treatment was delayed by 1 week. The patient returned a week later and was correctable to 20/20 with refraction. After the light treatments with both eyes, he is UCVA 20/20 for distance and J1 for near, and overall he was very happy with his refractive result. ■









