At our practice, the entire team plays an important role in educating the patient about options for cataract surgery, as well as determining who is a good candidate for a presbyopia-correcting intraocular lens (PC-IOL). Our technicians and staff are well informed about the various packages and IOLs we offer, and they play an active role in learning about the patients’ goals and discussing potential options with them. First, the technician who performs the testing may write notes about the testing for the workup technician and surgeon, such as “interested in being glasses-free,” or comments about the quality of the biometry obtained (eg, “1+ distortion”). Next, the workup technician performs a thorough examination and presents the objective testing data to me, as well as subjective feedback about the patient. This same technician will also be the scribe when I examine the patient and then finish scheduling the patient for surgery after I leave the room. This system works very well—the patient feels a connection with the technician, who knows them well, rather than being passed around; the technician is engaged and motivated to know the patient from start to finish; and I receive invaluable information about the patient’s personality and goals from an individual who has spent time with the patient.
Narrowing Down the Options
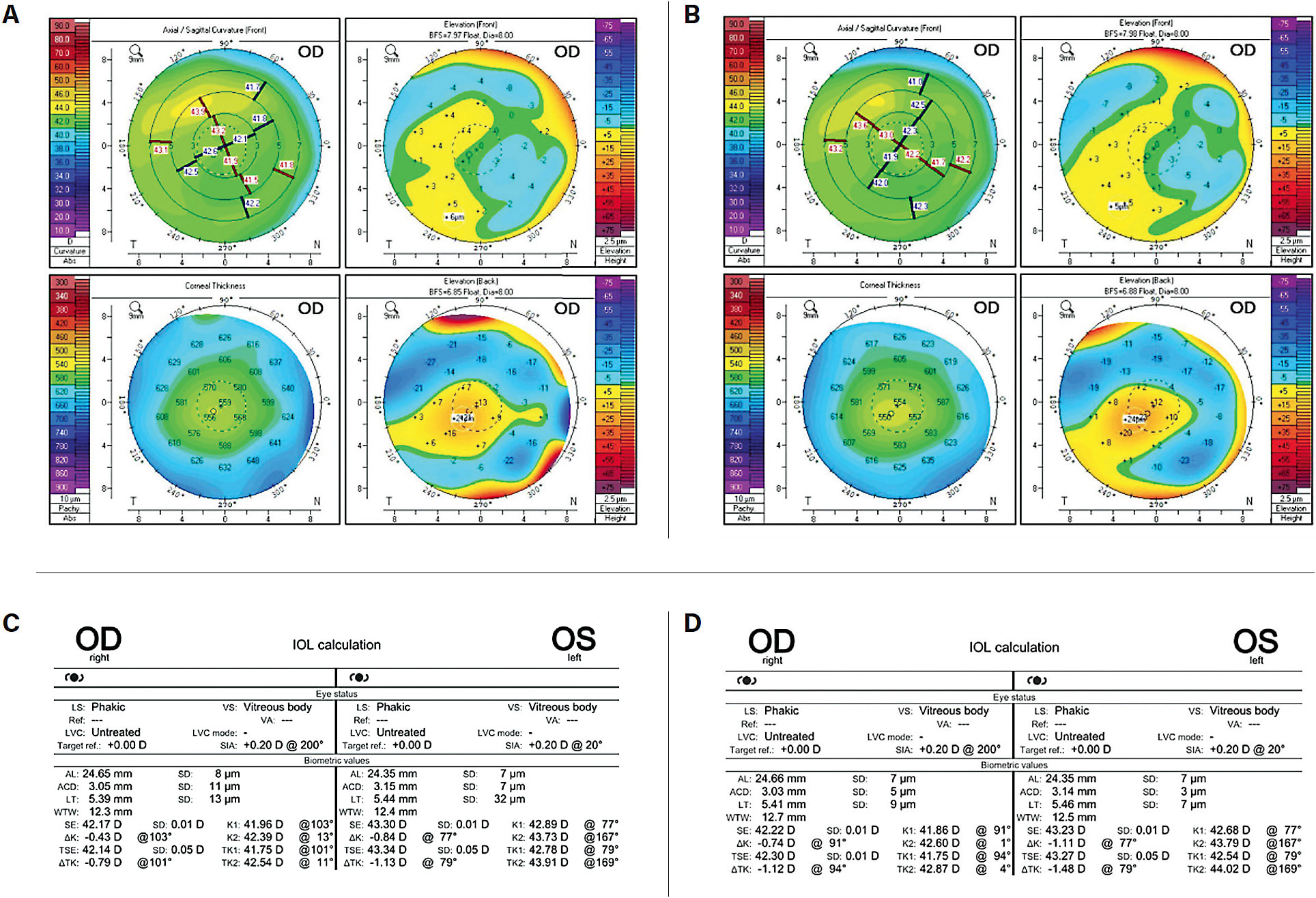
Based on the technician’s presentation and the objective data, I have often narrowed down my IOL choices for the patient before I even walk in the room. For example, if the patient has significant irregular astigmatism or retinal pathology, they are not a good candidate for a multifocal lens.
When I speak to the patient, I first try to understand their baseline in terms of their current near and distance vision and with and without correction. Myopic patients are often unwilling to sacrifice their near vision at any cost. I also ask, “What are your top 2 or 3 priorities for what you hope to do without glasses after surgery?” I rarely discuss specific technologies or products. Instead, I keep the conversation with the patient focused on outcomes, and then I use what I know about their anatomy, test results, and goals to determine which IOLs will help them reach those goals. If I have more than 1 option in mind, I might ask more questions, such as, “How do you feel about halos around lights at night? Would that bother you a little bit or a lot? Do you consider yourself a perfectionist?”
Toward the end of the consultation visit, I summarize the patient’s options: (1) glasses for all focal points; (2) distance vision without glasses; or (3) a full range of vision without glasses (assuming they are a candidate for all IOLs). Because terms like “near” can be vague, I try to put the IOL’s capabilities in terms that make sense to that individual. For a patient whose hobbies include painting, I might say, “If you choose distance only, you’ll be able to drive without glasses, but you’ll need reading glasses for painting.” Providing patients with information in context makes the tradeoffs more clear and relevant to their lives.
The Ocular Surface
The quality of the tear film and the health of the ocular surface are very important for postoperative success in terms of refractive error and quality of vision with presbyopia-correcting IOLs. Consequently, they factor heavily in my decision making.
When a patient has moderate to severe ocular surface disease, my preference is to first treat their dry eye, repeat the measurements at a later date, and then schedule surgery. I believe this approach is important for 2 reasons: (1) the patient understands that they have a separate problem that will exist after cataract surgery; and (2) I obtain more accurate biometry, leading to less residual refractive error.
I also warn my patients that dry eye can get worse in the immediate postoperative period; however, it will improve with time and diligence with their dry eye medications. I am very honest with my ocular surface disease patients that they must be committed to maintaining a healthy tear film in the long run; otherwise, they will not be happy. Research has shown that dry eye disease is one of the top reasons for dissatisfaction after cataract surgery with a presbyopia-correcting IOL, and this is not a simple issue to fix after the surgery has been performed. Rather, it is important to optimize the ocular surface as much as possible prior to any elective surgical procedure.
At our practice, we implemented a dry eye treatment protocol approximately 4 years ago, which has been extremely successful. All of our referring doctors have a 2-page Dry Eye Treatment Plan to hand to their patients, listing the various treatments available (including warm compresses, preservative-free artificial tears, prescription topical medications, ointments, in-office procedures, and more). The patient starts these treatments right away and before they see the surgeon for a consultation visit. We have thus seen a decrease in repeat biometry, and the patients understand that they have a separate chronic condition. Our enhancement rate after cataract surgery with multifocal IOLs has also decreased after implementing the Dry Eye Protocol.
Matching the Multifocal IOL to the Patient
My go-to approach for most patients with healthy eyes who want to be as glasses-free as possible is to use the “mix and match” approach. First, I operate on the dominant eye using an enhanced depth of focus (EDOF) lens, the Tecnis Symfony OptiBlue (Johnson & Johnson), because it offers outstanding distance and intermediate vision while also preserving contrast sensitivity and minimizing dysphotopsias. However, the patient may not have the ability to read small print with this lens, which is why I like to use the hybrid EDOF-multifocal (Tecnis Synergy) in the nondominant eye. This combination, in my experience, combines the advantages of each lens to best meet the patient’s goal of seeing well at distance, intermediate, and near. I tell every patient that they will have halos and that they should not expect good reading vision until the second eye has undergone surgery. For patients with a history of corneal refractive surgery, I like the Light Adjustable Lens (LAL, RxSight). For patients with history of previous radial keratotomy or with significant, irregular astigmatism, the Apthera IC-8 lens (Bausch + Lomb) is a fantastic choice. For patients who often drive at night, and do not want any halos, I will offer the LAL or an enhanced monofocal (Tecnis Eyhance).
For the surgeon, cataract surgery is a quick, routine operation. For our patients, treatment determines the vision they will live with for the rest of their lives. For their sake, it is important that we understand what our patients want and expect, do our best to deliver that outcome, and be absolutely honest about what our technologies can and cannot accomplish. ■









