Multiple strategies have been employed over time to mitigate the effect of presbyopia, the progressive, age-related loss of accommodative ability. These strategies include both surgical and nonsurgical options designed to increase depth of focus (DOF) at the monocular or binocular level. Nonsurgical monocular approaches include eyeglasses, multifocal contact lenses, and miotic eyedrops, while surgical solutions may incorporate accommodating, pseudoaccommodating, or small aperture intraocular lenses (IOLs), or even multifocal corneal refractive surgery. Surgical and nonsurgical binocular approaches may consist of bilateral application of these monocular solutions, e.g., bilateral implantation of multifocal IOLs, or they may leverage the binocular summative ability of the visual system via monovision, i.e., planned anisometropia via an emmetropic dominant eye and a near-targeted nondominant eye. As can be seen by the sheer number and variety of these approaches, no single technique has emerged as the ultimate, “one-size-fits-all” solution. Each method has advantages and disadvantages, which must be carefully weighed on a case-by-case basis before selecting each patient’s final strategy.
Monovision carries the advantage of avoiding the potential image quality and contrast sensitivity sacrifices inherent to the multifocal optics of pseudoaccommodating IOLs. However, monovision requires the patient to tolerate a certain level of anisometropia and suppress the perception of blur from the eye defocused with respect to the object of regard. In general, monovision success appears to be dependent upon on a well-focused distance eye with minimal residual refractive error and a nondominant eye targeted between -1.00 to -2.00 D.1,2 As we attempt to hit the anisometropia “sweet spot,” we strive to balance intermediate and near functionality with potential sacrifices to binocular image blur and loss of stereoacuity. One method used to increase DOF and minimize the aforementioned sacrifices has been to incorporate spherical aberration into the optics of the visual system.
Spherical Aberration
In geometric optics, spherical aberration (SA) refers to the variation in focal length seen as light rays transition from the paraxial to the peripheral regions of an optical system. The sign of SA provides information into the relationship between the paraxial and peripheral rays. In positive SA, peripheral rays are focused anterior to paraxial rays with the opposite relationship seen in negative SA (Figures 1a and 1b). In the case of (+) SA, as the object of regard approaches the eye, its corresponding image will proceed along the visual axis toward the retina, with paraxial rays coming into focus first, followed by peripheral rays (Figure 1c). Conversely, in (-) SA, peripheral rays will be focused initially, with paraxial rays to follow (Figure 1d). DOF can be achieved with both (+) and (-) SA since some aspect of the image will remain in focus as objects travel between these 2 focal points.

The mean SA of the virgin human cornea is positive, with a magnitude of approximately +0.28 µm (over a 6-mm pupil).3 When we are young, the SA of the lens is negative and counters that of the cornea, suggesting that visual performance is optimal at lower levels of total SA. As we age, the SA of the lens changes, with progressive loss of compensation for the cornea’s (+) SA, but lenticular SA is removed with cataract extraction. Early IOL models were typically designed with spherical anterior and posterior surfaces, which created IOLs with (+) SA that was additive to that of the cornea. Current IOLs are produced with spherical aberration levels tailored to the philosophy of the manufacturer. Some IOLs, such as the Johnson & Johnson Tecnis platform or the Alcon Clarion and Acrysof-IQ platforms, incorporate higher levels of negative SA, ranging from -0.27 to -0.21 µm, and are designed to reduce the eye’s total SA and improve overall visual quality. Other IOL platforms, such as the Bausch + Lomb Envista and Sofport, are manufactured with zero SA in efforts to balance the visual quality improvement seen with reduction of (+) SA and the sensitivity to decentration seen with IOLs containing higher levels of (-) SA. These factors must be considered if one wishes to harness SA to increase the visual system’s DOF.
The Light Adjustable Lens
The Light Adjustable Lens (LAL; RxSight) is a monofocal IOL that can be adjusted postimplantation via targeted irradiation with ultraviolet light using RxSight’s proprietary Light Delivery Device (LDD). The LAL is available in powers ranging from +4 to +30 D, with a spherical adjustment range of -2 to +2 D and a cylindrical adjustment range of -0.5 to -3 D (both in 0.25 D increments). The IOL can be adjusted 3 times and requires 2 lock-in treatments. In patients desiring spectacle independence, LAL implantation can be combined with monovision, and allows for contact lens simulation of true pseudophakic monovision, as well as near-target titration. The LAL is designed with (-) SA prior to treatment, and additional (-) SA (-0.06 µm for a 4.7-mm pupil) is induced with the first LDD treatment if the targeted refraction is between -0.5 and -2.25 D, and no flattening is induced in any meridian. The overall goal is to overcome the (+) SA of the cornea and leave the eye with (-) SA, with the intended effect of expanding DOF.
Changes in Spherical Aberration
Using the VAO adaptive optics wavefront aberrometer and vision simulator (VOptica), we recently measured the effect of spherical aberration induction on the visual performance of pseudophakic eyes.4 Spherical aberration was induced in eyes implanted with monofocal, extended DOF, or continuous range-of-vision IOLs, and varied from -0.13 to +0.13 µm for a pupil size of 4.5 mm, which is the aperture limit of the VAO. For comparison, this SA range corresponds to -0.4 to +0.4 µm for a 6-mm pupil, which is the most common pupil size referenced in the literature. In this study, we found that high contrast distance-corrected near visual acuity (DCNVA) improved by 0.13 logMAR (approximately 1 to 1.5 lines) with SA of -0.13 µm and worsened by 1 line with an equivalent level of (+) SA, supporting the potential for (-) SA to increase DOF in eyes with monofocal IOLs.
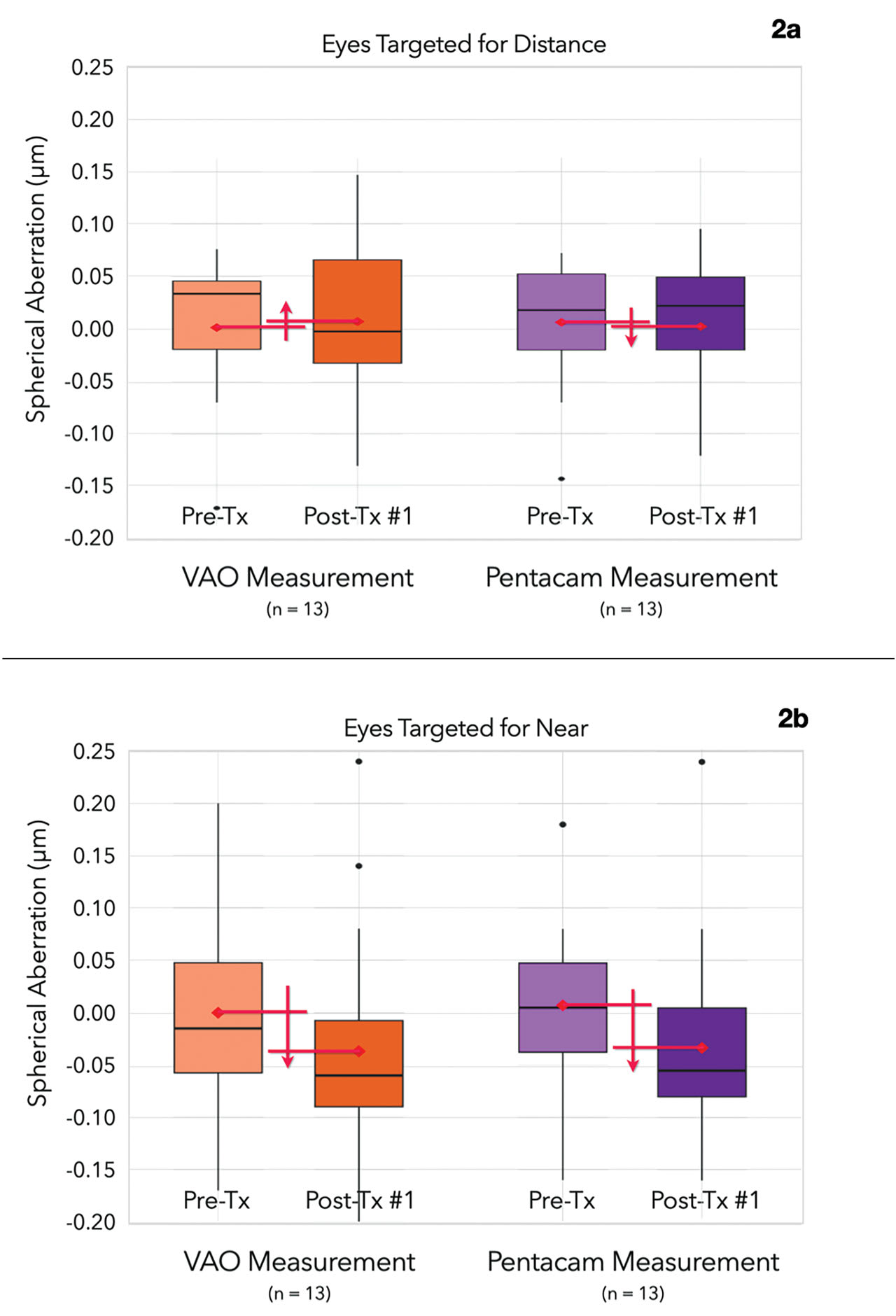
With this point in mind, we decided to examine the changes in SA and its effects on intermediate and near vision following LAL treatment in eyes targeted for uncorrected distance or near vision.5 In this study, we measured SA before and 1 week after the first LDD treatment using both the VAO and the Pentacam AXL-Wave (Oculus). We also measured the changes in monocular, high-contrast distance-corrected intermediateand near visual acuity (DCIVA and DCNVA) using the VAO. We found that the level of (-) SA induced by the first LDD treatment matched the expected level, with no significant changes seen in distance-corrected eyes and a significant increase of approximately -0.05 µm in the near-corrected eyes (Figure 2a and b). In addition, the level of induced (-) SA did not vary with the magnitude of refractive treatment. Slight increases in both DCIVA and DCNVA (0.8 and 0.4 lines, respectively) were seen in near-corrected eyes following LDD treatment compared to distance-corrected eyes. These results also support the potential for (-) SA to increase DOF in near-targeted eyes following LAL implantation and treatment. This DOF extension may permit a reduction in the targeted level of anisometropia in monovision patients, potentially improving binocular distance visual acuity and stereoacuity.
RxSight recently took this concept one step further with its introduction of the LAL+. The LAL+ is similar to the standard LAL in most respects but it includes a small central area of increased lens power, which provides slightly greater DOF even before any LDD treatments (Figure 3).
This modification appears to shift the defocus curve in the myopic direction, improving DCNVA by approximately 1 line. Negative SA is also added with the first LDD treatment of the LAL+ if the parameters satisfy the previously mentioned criteria. RxSight currently recommends bilateral implantation. However, some clinicians may lean toward using the LAL+ in the nondominant near eye and a standard LAL in the dominant distance-targeted eye. Early results appear promising, but more clinical experience will be necessary to fully define the optimal role for the LAL+, particularly its suitability in eyes with aberrated corneas.
Several questions remain as we explore the utility of the LAL in our monovision cataract surgery patients. The first may be “What is the best way to measure visual performance?” While we were able to demonstrate modest improvements with induction of (-) SA in monocular DCIVA and DCNVA, binocular through-focus visual acuity assessment may be a better way to measure true visual performance.6 In addition, we know that pupil size, corneal asphericity, and other higher-order aberrations can each play a role in fostering pseudophakic pseudoaccommodation. Currently, however, their contributions are poorly understood at the individual patient level. As our experience grows, we should be able to further optimize use of the LAL, extending our patients’ DOF while minimizing the impact of anisometropia on visual acuity and depth perception.
References
1. Durrie DS. The effect of different monovision contact lens powers on the visual function of emmetropic presbyopic patients (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2006;104:366-401.
2. Hayashi K, Yoshida M, Manabe SI, Hayashi H. Optimal amount of anisometropia for pseudophakic monovision. J Refract Surg. 2011;27(5):332-338.
3. Wang L, Dai E, Koch DD, Nathoo A. Optical aberrations of the human anterior cornea. J Cataract Refract Surg. 2003;29(8):1514-1521.
4. Kozhaya K, Kenny PI, Esfandiari S, Wang L, Weikert MP, Koch DD. Effect of spherical aberration on visual acuity and depth of focus in pseudophakic eyes. J Cataract Refract Surg. 2024;50(1):24-29.
5. Weikert MP, Kozhaya K, Wang L, Koch DD. Magnitude and visual effect of negative spherical aberration induction following treatment of the Light Adjustable Lens. American Society of Cataract and Refractive Surgery Annual Meeting 2024, April 7, 2024.
6. Zheleznyak L, Sabesan R, Oh JS, MacRae S, Yoon G. Modified monovision with spherical aberration to improve presbyopic through-focus visual performance. Invest Ophthalmol Vis Sci. 2013;54(5):3157-3165.
Disclosures
Dr. Weikert is a consultant for Alcon Labs, Carl Zeiss Meditec, and Heidelberg Engineering, and receives research support from Epion Therapeutics.