The pinhole concept is a basic optical principle in which the effect of paraxial rays is minimized by a small aperture, reducing the circle of blur in an optical system. In the human eye, a pinhole minimizes the effect of higher-order aberrations (HOAs), specifically spherical aberration, enhancing depth of focus and reducing the effect of refractive error. Its use in eye care is not new—slit or pinhole glasses can be traced back centuries, as early as the sixth century AD.1 In the clinical setting, we routinely use this concept diagnostically as a rough screen for pathology. We are now beginning to hone the capabilities of small apertures in the surgical world and are seeing impressive results with the FDA-approved IC-8 Apthera intraocular lens (IOL) (Bausch + Lomb).
Managing HOAs is of utmost importance in refractive surgery. Patients with history of radial keratotomy (RK), keratoconus, or corneal opacities especially have a greater propensity for HOAs, which can have significant effects on visual outcomes. There are various surgical techniques aimed at minimizing aberrations. However, with the renaissance of small-aperture optics, we have another tool in our toolbox for these patients. In our clinic, patients with prior RK have done especially well with the IC-8. We have seen fluid depth of focus with excellent uncorrected distance visual acuity (UCDVA)/uncorrected near visual acuity with little perceived contrast reduction. Plus, the pinhole mutes much of the diurnal refractive fluctuation that most RK patients deal with day to day.
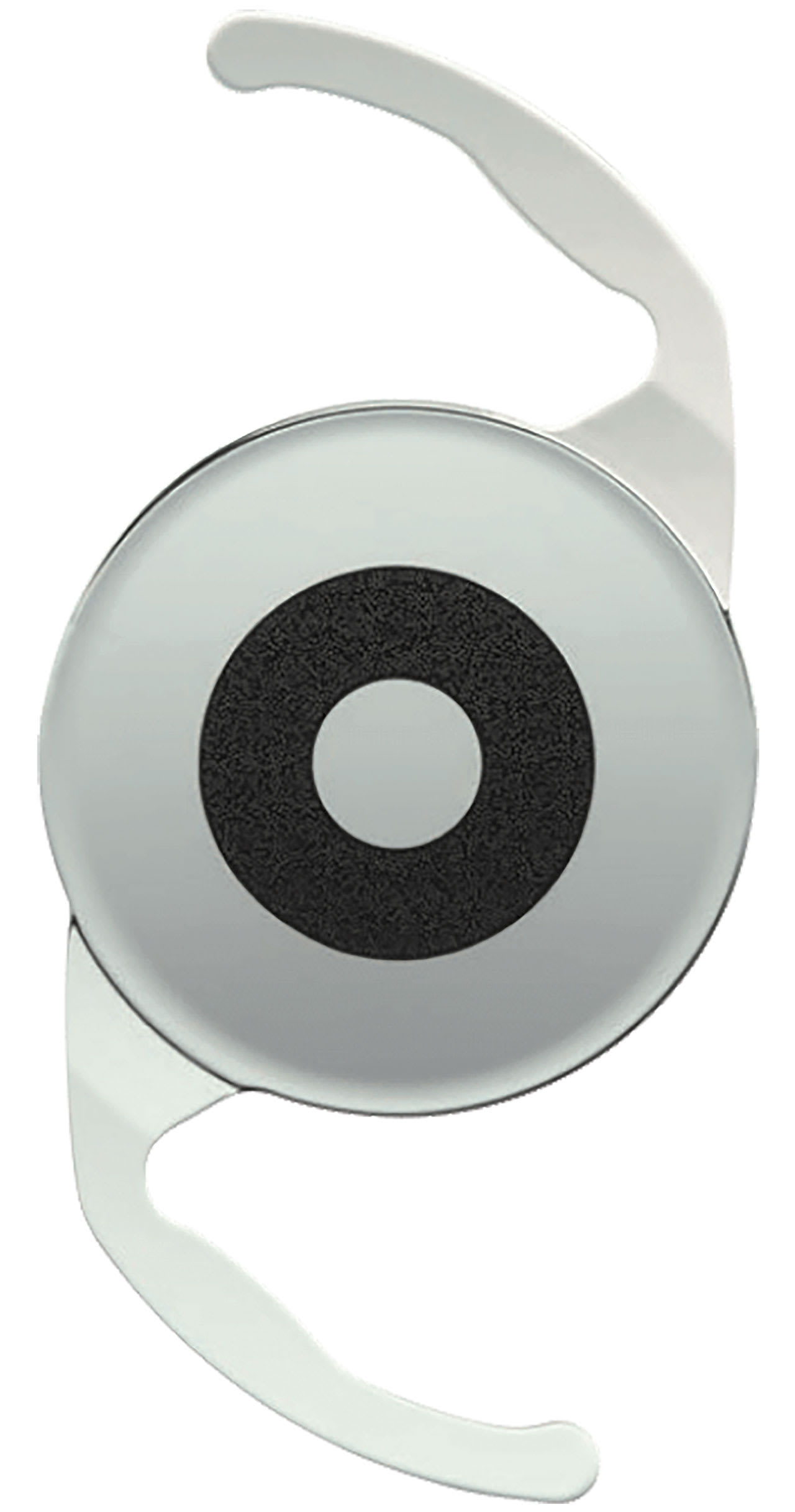
The IC-8 is not exclusively for those with compromised corneas. It is a solid option for presbyopic patients looking for relief from reading glasses. Many are likely familiar with corneal inlays as a refractive surgical option for presbyopes, notably the Kamra inlay. Inlays showed promise by enhancing depth of focus, yet complications arose in the form of refractive shifts, corneal haze, and reduced best-corrected visual acuity.2,3 While they still are used on occasion, they have grown out of popularity in recent years. The IC-8 design is similar; however, the difference is its placement at the eye’s nodal point and preservation of the cornea. The IC-8 is meant to be used in the nondominant eye, targeted for -0.75 D, while the fellow eye is implanted with a plano-targeted monofocal IOL. The -0.75 target broadens the defocus curve to comfortable lengths. Unilateral implantation is recommended due to possible loss of contrast sensitivity. However several surgeons have noted success with bilateral implantation in certain scenarios. Even with the slight myopia in the IC-8 eye, we are seeing in our practice that patients’ UCDVA is remarkable, often 20/25 in that eye or better with the added benefit of near vision. While monovision contact lens patients are obvious candidates for this IOL, the term “monovision” is misleading. Given the fluid depth of focus in the IC-8 eye, matched with a precisely plano-targeted fellow eye, patients retain comfortable binocularity without common symptoms of severe anisometropia. Hitting a plano target in the dominant eye is critical, while the near-set nondominant IC-8 eye has a much wider landing zone. For this reason, we often use a Light Adjustable Lens (RxSight) in the fellow eye or will at least correct even small amounts of astigmatism at the cornea with laser-assisted astigmatic keratotomy.
Speaking of aberrations, we cannot forget about astigmatism. The IC-8 is indicated for patients with up to 1.5 D of corneal astigmatism.4 This indication comes in handy when it is difficult to pinpoint the exact axis. With traditional surgical astigmatic correction, nailing the steep axis is key for refractive accuracy. With the IC-8, the corneal cylinder is very well masked. It is important that patients have a dilated pupil size of at least 7 mm. Postoperatively, performing a dilated exam is very difficult through the central hole. Therefore, peripheral retinal examinations must be performed outside of the 3.23-mm outer aperture diameter. It is also important to keep in mind that autorefraction and retinoscopy measurements will be unreliable with this lens. Subjective refraction yields a much softer end point, meaning that patients tend to tolerate higher levels of blur. Usually my refractions are a “midpoint” between just noticeable differences in blur. Another option is using a red/green balance test. After performing a subjective manifest refraction, ask the patient which side is clearer: the red or the green. If they respond with the red, add 0.25 D of minus until each side is equal. The same goal can be accomplished adding 0.25 D of plus if they respond initially that the green is clearer.
As with any premium IOL, setting expectations is key. This is not the holy grail. Realistically, this IOL will provide a degree of spectacle independence. However, patients must be counseled that they will still need added help for small print or in low light. I describe this task as “functional reading vision”— reading glasses will certainly help, but a patient should not feel stranded if they do not have any handy.
References
1. Barnes RJ. The history of slit and pinhole glasses. Aust J Optom. 1932;15(6):34-38.
4. US Food and Drug Administration. Summary of Safety and Effectiveness. Hydrophobic Acrylic Small Aperture Intraocular Lens (IOL). 22 July 2022. https://www.accessdata.fda.gov/cdrh_docs/pdf21/P210005B.pdf
Disclosures
Dr. Bruns reports relevant disclosures including RxSight, Staar Surgical, and Glaukos.

Dr. Bruns is lead optometrist at Summit Eye Care in Milwaukee, where he serves as director of practice development. His clinical focus is pre-/postoperative care and ocular disease. He is also an adjunct clinical assistant professor at the Michigan College of Optometry.








